ASSESSING THE VIOLENCE RISK IN SUBJECTS WITH FORENSIC PSYCHIATRIC EXAMINATION
Abstract
Objectives: Assessing the violence risk in the population with forensic psychiatric examination is carried out subsequent to assigning the diagnostic, the discernment. Measuring the violence risk is concluded in the proposals of the board of forensic psychiatric expertise for actions of medical safety. The use of modern, contemporary tools to evaluate the violence risk (Guide for Assessing Violence, HCR-20) provides documentation on the factors which led to the conclusion of forensic psychiatric examination. Method: The purpose of the research is represented by the assessment of the violence risk in subjects examined within the Laboratory of Forensic Medicine from Bihor County between 2010 and 2011. In this respect, the following tools were employed: Mini International Neuropsychiatric Interview (MINI), the Guide of Assessing the Violence Risk (HCR-20), Psychopathy Checklist Revised (PCL-R), Clinical Global Impresion Severity (CGI-S). Results: The violence risk and relapse in the delinquent population diagnosed with personality disorder correlates with the stable demographic and historical factors (HCR- 20 subscale H). The clinical, dynamic factors (HCR-20 subscale C) involved in violence are predominantly associated with psychotic disorders and schizophrenia. The severity of the psychosis, the severity of violence, the adherence to treatment implies the recommendation for measures of medical safety. Conclusions: HCR-20 has inter-rater validity within the population studied. HCR-20 items don't have the same importance and the same predictive power for violence or relapse. HCR-20 doesn't offer cut-off scores to indicate the degrees of the violence risk, but founds and increases the transparency of the recommendation made by the board of forensic psychiatric expertise.
INTRODUCTION
At the level of the European Union, the forensic psychiatric examination in subjects with delinquent behavior uses tools of assessing the violence risk and the risk for relapse. EMLP differs from a country to another according to legislation, medical organization and judicial framework. Analyzing the legislation of the member states of the European Union, Salize and Dreβing state that in
2005 “a reconcilability of the legislative concepts along the European borders seems to be presently difficult to obtain. At least the elaboration and implementation of training standards for specialists in forensic psychiatry are desirable”(1).
The established tools (HCR-20, PCL-R) in the forensic practice had been adapted on various samples (delinquents, penal convicts, patients with mental disorder from the community and the forensic psychiatric structures). The use of these tools on the Romanian population needs validation, evaluators’ training, and establishment of some national norms for the employment in forensic assessments. The capacity of the tools to differentiate various degrees of violence risk (mild, medium, high), to frame categories is indicated to be correlated in the case of individuals with forensic psychiatric evaluation with the recommendations for measures of medical safety.
The notion of assessing the violence risk (Mills et alii, 2011) includes: a) determining the level of risk; b) identifying the significant factors which contribute to the risk; c) identifying some management strategies for reducing the risk; d) communicating the information about the risk within justice (2).
OBJECTIVES
Measuring the violence risk with contemporary tools of forensic evaluation (HCR-20, PCL-R) was the main purpose of the research. The HCR-20 analysis for inter-rater validity in subjects with forensic psychiatric expertise, the identification of factors involved in violence acts in relation to its severity and the evaluations and recommendations of the forensic experts are themselves objectives followed in the present research.
MATERIAL AND METHOD OF RESEARCH Participants
The research comprises 137 subjects with forensic psychiatric evaluation within the Laboratory of Forensic Medicine of Bihor County between January 2010 and December 2011. Subjects diagnosed with mental retard with no penal actions, examinations for legal competence, driving and gun licence at request were excluded from the research.
Tools
The data used in the research were collected from the forensic psychiatric evaluation, which includes: the psychiatric interview, the psychological examination, the electroencephalogram, the access to the medical and penal records. Complementary, MINI (3), CGI-S (4), HCR-20, (5), PCL-R (6, 7) were exploited.
The psychological evaluation carried out by the clinician psychologist was adapted to the type of subject evaluated, comprising projective and personality tests, the IQ assessment by the method of Progressive Matrices Raven and/or Wechsler Adult Inteligence Scales (WAIS).
The subjects were examined by the author, along with the members of the expertise board with the agreement of the Laboratory of Forensic Medicine Bihor. The collection of data for the study, the specific evaluations (the MINI interview and conclusion) didn’t interfere with the forensic decision. The diagnosis was formulated according to the International Clasification of Diseases variant 10, ICD 10.
The Description of Tools
HCR-20 (Webster, Douglas, Eaves & Hart, 1997) is the tool frequently used in the clinical evaluation of violence risk. HCR-20 comprises a list of 20 items, considered by the authors as being factors involved in the violent behavior of delinquents with or without mental disorders. 10 items of the HCR-20 are historical, demographic, stable; 5 items refer to the clinical symptomatology and 5 items to risk factors. Items are rated as absent, possibly present and definitely present. HCR-20 intends to be an “aide memoire” which assures the clinician of having taken into account most factors concerned in violence. The use of HCR-20 on Romanian population is easy owing to the overlapping of items with the practised psychiatric evaluation. The appreciation and the management of violence by the psychiatrist on longer or shorter periods is a permanent necessity of the clinical activity.
Psychopathy Checklist Revised (PCL-R, Hare, 2001) is a standard tool for assessing psychopathy, defined and conceptualized by Hare. It contains 20 items and was validated on delinquent males, penally convicted. It proved to be a good predictor for relapses with or without violence (6, 7).
MINI (Mini International Neuropsychiatric Interview) was employed for establishing the diagnostic, especially the dissocial personality disorder, by section “P”. MINI is validated on Romanian population; its use lasts for about 15–20 minutes. The diagnostic accuracy is tantamount to that of the Structured Clinical Interview for (SCID) and the Composite International Diagnostic Interview (CIDI) of the World Health Organization.
The socio-demographic data used in the research were obtained by adapting the items of some European s o c i o – d e m o g r a p h i c i n v e n t o r i e s ( C l i e n t S o c i o – Demographic and Service Receipt Inventory – European Version, CSSRI-EU) (8).
The forensic history, the existence of the criminal record, was fetched by analyzing the data of the penal file, accessible to the forensic psychiatric expertise board.
The penal act for which the subject is examined is defined in relation to the severity of violence: mild, medium, severe (mild – verbal violence, hostility, threat; medium – beating, robbery; severe – homicide, sexual offence, use of armes blanches/ knuckles or fire arms, beating which endangers one’s life. The penal acts without violence were considered as being the theft, the gross indecency, false witness, the destruction of material goods.
The data obtained were statistically analyzed with IBM SPSS 20 (a pack of statistical programmes for social sciences, version 20) for Windows.
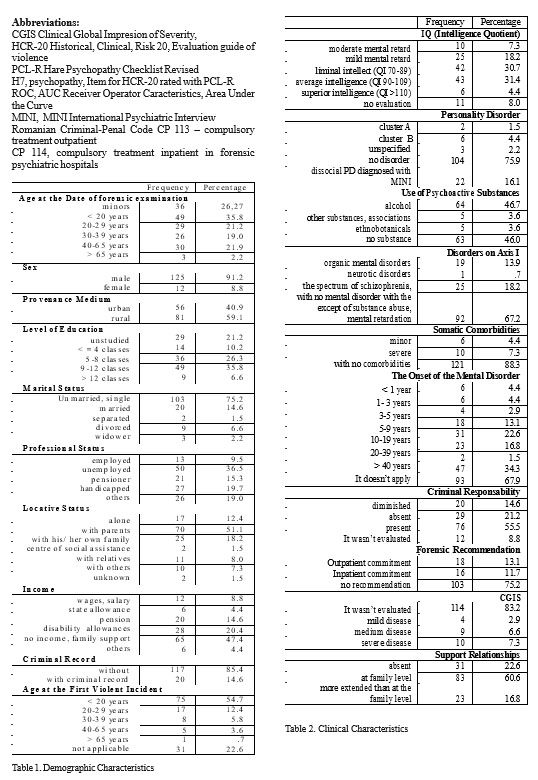
The demographic data of the 137 subjects examined as to percentage and frequency are presented in Table 1, and the clinical characteristics in Table 2.
The analysis of the socio-demographic data reveals that in the group studied male adults are predominant: 125 subjects (91.2%), 81 (59.1%) are from the countryside, 43 (31.4%) have reduced education, with at most 4 primary classes, 103 (75.2%) are unmarried, 70 (51.1%) live with the parental family, 50 (36.5%) are unemployed, and 65 (47.4%) have no income.
The age of the first violent incident is with most of the subjects (67.1%) under 30 years. The level of education and the low social integration are in compliance with the reduced index of intelligence. The mental retardation and the borderline intelligence are present in 77 subjects (56.2%).
Major mental disorder from the schizophrenia spectrum disorder and other psychoses are diagnosed in 25 subjects (18.2%).
The distribution of the severity of the examined subjects’ act is similar to that encountered in other national forensic populations, the offence without violence being identified in 76 subjects (55.5%) (9). The most frequent offence without violence was the theft, present in almost 50% of the examined subjects.
The psychiatric diagnostic was established in forensic psychiatric evaluation and by personal evaluation; the assessment tool used was MINI. In the studied sample the following psychiatric disorders were identified:
a) Organic mental disorders (F00-F09, after ICD 10):
13.9% (19 subjects);
b) Psychotic disorders, disorders from schizophrenia spectrum disorders (F20-F29), mood disorders (F30- F38): 18.2% (25 subjects);
c) Neurotic disorders (F40-F48): 0.7% (one subject);
d) Personality disorders (F60-F69) from Cluster A are present in 1.5% of the subjects (2 subjects), from Cluster B in 4.4% (6 subjects), unspecified personality disorder in 2.2% (3 subjects). The tools of evaluation used (MINI) revealed: dissocial personality disorder in 16.1% of cases (22 subjects), diagnostic which was not established by the f o r e n s i c p s y c h i a t r i c e x a m i n a t i o n b o a r d . H a r e psychopathy (score PCL-R > 25, item H7-HCR-20 = 2) is present in 8% (11 subjects). In the studied sample, the diagnostic of personality disorder (H9-HCR-20 =2) is present in 17.5% (24 subjects). The analyzed sample illustrates a reduced proportion of Hare psychopathy than of personality disorders; as at the HCR-20 rating they don’t coincide, they don’t overlap. At the partial rating of itmes H7 and H9 these overlap as personality traits. The globally adopted taxonomies (DSM and ICD) don’t include psychopathy as established by Hare (6, 7).
e) Disorders related to the use of psychoactive substances are reflected in the H6 item; the collection of data was done in order to identify the type of substances implied as well. Addiction to substances like benzodiazepine, caffeine and nicotine was not processed.
Somatic comorbidities were less frequent, being present in 7.3% (10 subjects), fact which can be explained by the relatively young age.
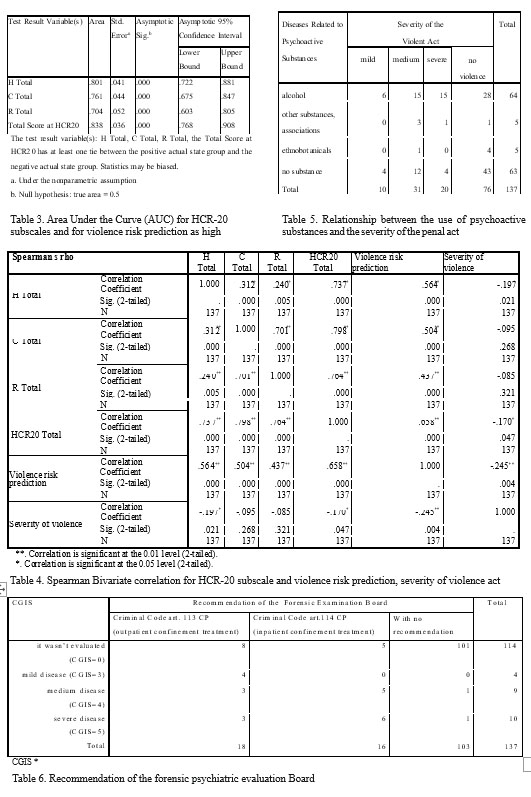
Results regarding the HCR-20 Tool Out of the 137 subjects, 62 were evaluated by two psychiatrists with clinical experience in the forensic psychiatry, one of them being the author himself. The HCR-20 was rated for the analysis of the inter-rater reliability by calculating the Crombach alpha coefficient. Crombach alpha indices obtained have significant values (for total H – 0,9069; total C – 0,8698; Rtotal – 0,8698), framing within the optimum interval. The concordant results are explained by the access to the same pieces of information, the same clinical experience, the same training.
The HCR-20 predictability was analyzed by the method Receiver Operator Characteristics, Area Under the Curve (ROC-AUC). The HCR-20 subscales were analyzed in relation to the prediction of the high violence risk (Chart 1, Table 3).
Chart 1(AUC for HCR-20 subscales and prediction of violence risk as high) When predicting a degree of high violence risk, AUC significantly correlates with HCR-20. When predicting a degree of low or medium risk, ROC-AUC doesn’t correlate more than the chance (when AUC = 0.5) with HCR-20. In conclusion, the ROC-AUC curve doesn’t illustrate the same response for predicting the low, medium and high violence in the heterogeneous studied sample (subjects with major mental disorders without discernment, with mental disorder with discernment, with no psychiatric diagnostic). The prediction provided for a one-year’s period.
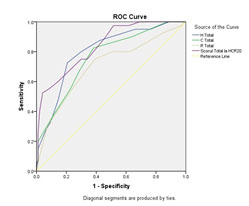
Chart 1. The HCR-20 subscales were analyzed in relation to the prediction of the high violence
Results regarding the Analyzed Population
The severity of the violence act and the prediction for violence were analyzed and correlated in terms of HCR-20 subscales. The results obtained were statistically elaborated by Spearman bivariate correlations. (Table 4)
H, C and R subscales and the HCR-20 total score significantly correlate with each other with the prediction of violence risk, namely with the final judgment of the risk (low, medium, high) assisted by HCR-20.
The H subscale and the HCR-20 total score negatively correlate with the severity of the act for which the expertise is carried out.
Previous violence (HCR-20, H1) was identified as follows: absent with 25 subjects (18.2%), possible with 49 (35.8%) and present with 63 (46.0%); mean = 1,28; standard deviation = 0.755. The possibility to rate with 1 the items of HCR-20 scale for the possible or partially present factors can be noticed. We underline the context of a single evaluation of the examined subjects and the limited time as causes which hindered the rating of absent or present. H1 correlates with the prediction of the violence risk but not with the severity of the act for which the expertise is carried out. The explanation is the manner of defining the act, serious dissocial actions without violence being considered the following: destruction of goods, theft and home infringement. Verbal, physical violence and threat are frequently associated with this behavior, but, as a rule, they are not registered in the medical documents of justice.
The H5 item refers to disorders connected with the use of psychoactive substances. We underline that disorders related to the use of psychoactive substances i n c l u d e a l s o d i s o r d e r s p r o d u c e d b y a l c o h o l , ethnobotanicals, and association of substances which include alcohol, ethnobotanicals and psychodysleptics. The consumption of ethnobotanicals was revealed in 5 subjects (3.6%) and of alcohol in 64 (46.7%). The alcohol use is correlated with the prediction of violence risk and the severity of the violent act. Table 5 illustrates the relationship between the use of psychoactive substances and the severity of the penal act.
The clinical diagnostic of psychopathy established by PCL-R is supported by the H7 item; for rating, a threshold rate of 25 points was employed, accepted in the literature for the European population (Hare, 2001). In the group studied, psychopathy (Hare) is present in 8% of the examined subjects (11 subjects), average = .48, standard deviation = .643. 32,1% of the subjects have traits of Hare psychopathy and personality disorder (rated by H9 item). Partial rates for the H7 item for psychopathy (32.1% – 44 subjects) and H9 for personality disorder (47.4% – 65 subjects) were obtained also due to the inclusion of the minor subjects examined in a number of 36 (26.27%). The diagnostic of Hare psychopathy and personality disorder were defined only after the age of 18.
The H9 item supports the diagnostic of personality disorder according to ICD-10 and DSM-IV. The diagnostic of certainty is established at a rate of 2 of the HCR-20, a rate of 1 indicated a possible personality disorder or traits of personality disorder and a score of 0, the absence of personality disorder. The HCR-20 rating establishes a dimensional diagnostic of personality disorder, the diagnostic of certainty being later determined either previously, diagnostic taken from the medical records, either by the evaluation of the forensic examination board or by personal evaluation.
CGIS measured the severity of psychotic disorders from the schizophrenia spectrum disorder and mood disorders at the moment of the expertise, but not at the moment of the action, the severity being often the same. The hypothesis that CGIS is a global indicator correlated with violence, the prediction, the safety measures recommended by forensic psychiatric examination board are verified, the rate of chi square being significant (87.967 Pearson Chi-Square 0.000). Table 6 shows significant correlations between CGIS and the recommendation of board. A CGIS scored with 4 (obvious symptomatology but with modest functional effects or distress) or 5 (the symptoms significantly modify the occupational or social activity or causes a severe level of stress) defined the threshold of decompensating psychoses.
At the studied sample, the base rate is reduced for severe violence in schizophrenia (n=2; 10%) compared with severe violence in other mental disorders, in organic mental disorders (n=3; 15%), in dissocial personality disorder (n=8; 4%), alcoholic dependence sindrom or co- morbidity (n=15; 75% ), with no psychiatric diagnostic of major mental disorder (n=15; 75%), subjects with disorders in which they have discernment and responsibility and were included in reformatory structures.
DISCUSSIONS
The use of modern, contemporary tools (HCR- 20, PCL-R) provides information about the risk factor for violence and relapse in the population with forensic psychiatric expertise.
Assessment the violence risk is concluded within the recommendation of the forensic experts for measures of medical safety. Although the use of these tools on the Romanian population needs validation, their ability allowed the identification of factors involved in violence in relation to its severity. The age of the first violent incident is under 30 with most subjects. (10)
The repartition of the severity of the act done by the subjects examined within the Laboratory of Forensic Medicine from Bihor County (2010–2011) is similar to that encountered in other national forensic populations, the expertises carried out at the Psychiatry Hospital and for Safety Measures Sapoca (9) both for non-violent acts 55.5% versus 44.3% and for acts with severe violence 14.6% versus 13.1%, which include especially the homicide and sexual violence, the results being explained by the use of HCR-20 and its definitions for violence.
The HCR-20 predictability in our study doesn’t represent the same sensibility for the prediction of mild, medium and severe violence. The differences can occur due to the heterogeneous sample studied, the limited period of time and a single evaluation. The H subscale and the HCR-20 total score negatively correlate with the severity of the violence act examined.
The H1 item, considered to be the most important predictor of violence with delinquents, doesn’t correlate with the severity of the act for which the expertise is done, probably due to the manner of defining the act; highly dissocial acts which, as a rule, are not registered in the medical files and in those pertaining to justice (destruction of goods, theft, trespassing) are taken as non-violent. The HCR-20 rating (H7 and H9 items) establishes a dimensional diagnostic of the personality disorder, the clinical diagnostic being determined by PCL-R (the threshold score = 25).
CGIS measures the severity of psychotic disorders (from the schizophrenia spectrum and mood disorders), being a global indicator correlated with violence, the prediction and the safety measures suggested.
For the use of HCR-20 or other tools, studies on Romanian population, uniform training for all specialists in mental health, norms elaborated by the Ministry of Health are necessary. The inter-rater validity diminishes if there are inequalities in training or a different clinical background (social worker, psychologist, psychiatrist, psychology or psychiatry expert in forensic evaluation or in that of populations from correctional settings).
CONCLUSIONS
HCR-20 has an inter-rater validity on the population examined, reflected by the Crombach alpha index.The most important risk factors for violence are: previous violence (H1 item), abuse of psychoactive substances (H5 item), psychotic decompensation (CGIS greater or equal to 4 registers the affectation of social functionality).
PCL-R identifies variants of the dissocial personality disorder (psychopathy according to Hare, 8%), and MINI the disoccial personality disorders (16.1%), with a history of conduct disorders.
CGI-S correlates with the recommendation of the expertise medicolegal psychiatric board as important factor in the severity and evolution of schizophrenia.
Severe violence in schizophrenia has a low base rate compared with the population examined for penal acts in forensic psychiatric assessment.
The use of certain clinical tools for evaluating the violence risk in the psychiatric forensic population increases the transparency of the assessment, detailing historical and clinical factors, and the elaboration of the assessment in a descriptive manner of the risk and protective factors, the analysis of the contextual factors clarify the recommendation of the board.
REFERENCES
1. Placement and Treatment of Mentally Ill Offenders. Legislation and Practice in EU Member States, Central Institute of Mental Health, M a n n h e i m , G e r m a n y , H J S a l i z e a n d H D r e ß i n g . (http://ec.europa.eu/health/ph_projects/2002/promotion/fp_promotion_2002_frep_15_en.pdf) Retrived at 20 sep 2011.
2. JF Mills, DG Kroner, RD Morgan. Clinician’s guide to violence risk assessment. New York, London: The Guilford Press, 2011, 2.
3. Sheehan DV, Lecrubier Y, Sheehan KH et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;(59)Suppl 20: 22–33.
4. Guy W. ECDEU Assessment Manual for Psychopharmacology Revised (DHEW Publ No ADM 76-338). Rockville, U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration. NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs, 1976,218–222.
5. Webster CD, Douglas KS, Eaves D, Hart SD. HCR-20: Assessing the Risk for Violence (Version 2). Vancouver: Mental Health, Law, and
Policy Institute, Simon Fraser University, 1997b.
6. Hare RD. Manual for the Psychopathy Checklist-Revised (2nd ed.). Toronto: Multi-Health Systems, 2003.
7. Hart S, Hare R, Forth A. Psychopathy as a risk marker for violence: Development and validation of a screening version of the Revised Psychopathy Checklist. In: Monahan J, Steadman H (Eds.). Violence and mental disorder. Chicago, IL: University of Chicago Press, 1994, 81–98.
8. CSSRI – EU (EU Schizophrenia study). Final version: 15 September
1997 (http://www.dirum.org/assets/downloads/634462380166178864- CSSRI%20-%20EU.pdf) retrived at 26 aug 2011.
9. Moşescu M, Chiriţă R, Dragu M, Chiriţă V. Assessement and management of violence risk in Forensic Psychiatry. Rom J Leg Med
2010;(18): 289 – 294.
10. Costea G, Gheorghiu V, Buda O, Popescu I, Trandafir MS, Statistical association criteria in forensic psychiatry-a criminological evaluation of casuistry. J Med Life 2011;4(1): 21-9.
***



