SOCIAL AND ADMINISTRATIVE CHARACTERISTICS OF PATIENTS WITH ALCOHOL WITHDRAWAL IN A ROMANIAN SAMPLE
Abstract
Introducere:. Tulburările induse de alcool reprezintă o patologie psihiatrică frecventă. Nu există însă suficiente studii pentru a putea caracteriza complet acești pacienți din punct de vedere social și administrativ. O b i e c t i v e : A c e s t s t u d i u î ș i p ro p u n e s t u d i e re a caracteristicilor socio-administrative ale pacienților cu sindrom de sevraj la alcool într-un eșantion din România. Metode: Eșantionul include 2460 de pacienți diagnosticați cu o tulburare legată de consumul de alcool dintre care 888 au avut sindrom de sevraj în momentul prezentării la camera de gardă a Spitalului de Psihiatrie ,,Prof. Dr. Alexandru Obregia'' din București în perioada 1 ianuarie 2017-31 decembrie 2017. Rezultate: Dintre aceștia, 68,8% au fost diagnosticați la externare cu dependență de alcool și 31,2% cu consum nociv. 43% dintre pacienți s-au prezentat singuri la camera de gardă, iar cel mai frecvent diagnostic de internare a fost intoxicație etanolică. Dintre pacienții internați cu sevraj la etanol, 36,49% au dezvoltat sevraj complicat și 89,79% dintre aceștia au fost transferați de la alte unități spitalicești. Am aflat că pacienții care se prezintă cu sindrom de sevraj la etanol au avut durate de spitalizare mai mari, au fost de obicei transferați de alte unități spitalicești, nu au prezentat agresivitate la momentul internării iar jumătate nu au avut asigurare medicală. În plus, pacienții transferați au avut un risc mai mare de a dezvolta sevraj complicat comparative cu cei aduși cu ambulanța de la domiciliu sau cei ce s-au prezentat singuri. Concluzii: Există numeroși factori socio-administrativi care pot caracteriza un pacient ce se prezintă cu sevraj la etanol însă sunt necesare mai multe studii pentru a putea elucida complet gradul de implicare al fiecărui factor.
INTRODUCTION
Alcohol related disorders are some of the most frequent disorders diagnosed in psychiatric hospitals which also implies a higher cost of health services needed to treat them. One earlier study (1) showed that the cost per patient for detoxification from alcohol was between 3 319$ and 3 665$. A study (2) of 817 admissions in a hospital from Cluj reported an annual hospitalization cost for these disorders of about 562 794 Euros, ranking third in position after psychotic disorders and major depressive disorder. The World Health Organization (WHO) shows (3) that in the population of Romania the medium alcohol consumption was 10.4 L of pure alcohol per capita over 15 years old during 2008-2010, showing an increase in consumption compared to 2003-2005 when it was 8.8 L per capita. About 50% of the alcohol used is beer, followed by wine – 29% and spirits – 21%. The prevalence of alcohol induced disorders in both genders in 2010 was about 2.4% compared with the rest of WHO European region where the prevalence was 7.5%.
We already know some of the risk factors for developing alcohol withdrawal from literature (4) such as: frequency of abuse, quantity of alcohol drank, the presence of another medical disorder, family history and patient history of alcohol withdrawal, but the social and administrative factors are not yet fully understood. In addition, unlike other health care systems, in Romania, alcohol withdrawal is treated almost exclusively in psychiatric hospitals and therefore, we had access to the majority of patients with alcohol withdrawal, making the results of our research more generalizable.
The risk factors for developing complicated withdrawal (5-7) are: chronic alcohol use, history of delirium tremens, age over 30 years, presence of a somatic disease, presence of withdrawal symptoms in spite of a high blood alcohol level and a longer period of abstinence. Complicated withdrawal is defined as somatic (presented further) or psychiatric (delirium, alcoholic hallucinosis) consequences linked to imbalances caused by the withdrawal itself. Severe (or complicated) alcohol withdrawal syndrome is associated (8, 9, 10) with electrolyte and hydric imbalance which can lead to arrhythmias, seizures, cardiac insufficiency and rhabdomyolysis which at endpoint raise the risk of death in these patients.
In this article we will examine the social and administrative factors which are present in a Romanian sample of patients diagnosed with alcohol withdrawal. All this data can offer us a partial profile of a patient with alcohol withdrawal in order to raise caution when dealing with such cases and better understand which patients with alcohol related psychiatric disorders are at risk of developing alcohol withdrawal, which represents a serious medical emergency. Definitively more studies are needed for a more complex profile so that we can be able to better predict which patients will develop complications of withdrawal and what the best course of action is during hospitalization.
METHODS
A non-randomized observational retrospective study was conducted in the “Prof. Dr. Alexandru Obregia” Psychiatric Hospital with a data base of 19563 patients out of which 2460 met the diagnostic criteria of an alcohol use disorder and 888 of them were admitted with alcohol withdrawal during 01.01.2017-31.12.2017.
The data was compiled and analyzed using IBM SPSS Statistics 20. For the variables with abnormal distribution we used the Mann-Whitney U test and for the categorical values we calculated the frequencies and then we applied the Chi Squared test. P values below 0.05 were considered statistically significant. For this study we had the approval of the Ethics Committee of “Prof. Dr. Alexandru Obregia” Psychiatric Hospital.
RESULTS
From a total of 2460 patients included, 68.8% (n=1692) had, either a primary or a secondary, diagnosis of alcohol dependence and 31.2% (n=768) or of alcohol abuse. Of all patients, 42.93% (n=1056) came alone at the emergency room and the most frequent admission diagnosis was alcohol intoxication (53%, n=1308). The primary discharge diagnosis of alcohol related disorder represented 22.72% (n=559) of all the patients discharged in 2017 from “Prof. Dr. Alexandru Obregia” Psychiatric Hospital, being surpassed by personality disorders (26.3%) and major depressive disorder/recurrent depressive disorder (43.96%). Amongst the patients admitted with alcohol withdrawal syndrome, 36.49% (n=324) developed complicated withdrawal symptoms and 89.79% (n=265) of these were transferred from another hospital.
All the discharged patients often presented either psychiatric or non-psychiatric comorbidities like: alcohol dependence (n=1467, 59.63%), personality disorders (n=395, 16.05%), epileptic seizures (n=217, 8.82%), c e r e b r a l a t r o p h y ( n = 5 2 , 2 . 1 1 % ) , a l c o h o l i c polyneuropathy (n=85, 3.45%), type II diabetes (n=145, 5.89%), chronic hepatitis C (n=45, 1.82%), pancreatitis (n=28, 1.13%) alcoholic liver disease (n=799, 32.47%), vitamin B group deficiency (n=1106, 44.95%), hyperlipidemia (n=477, 19.39%), hydric and electrolytic imbalance (n=97, 3.94%), cardiovascular disease (n=61, 2.47%) and anemia of all causes (n=121, 4.91%).
Out of the total patients with alcohol withdrawal 70.27% were medically insured meanwhile only 55.55% of all the patients admitted with complicated withdrawal were ensured.
Our results showed that patients who presented complications of withdrawal syndrome spent more days in the hospital compared to patients without complications, representing a medium of 11 days compared to 8 days (p=.002, r=.219). The total admission number of patients presenting with alcohol withdrawal (Mdn=2) differed significantly from those who did not present with withdrawal (Mdn=5).
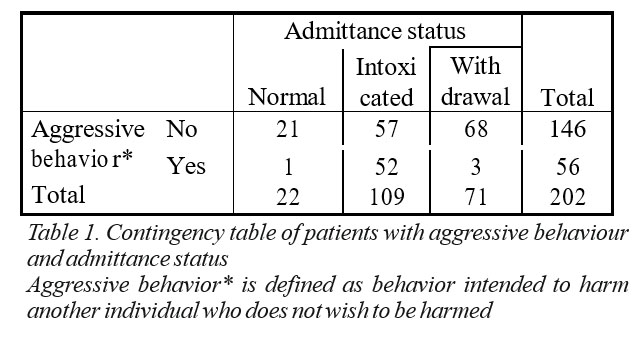
There was a 15.4 times higher risk of patients presenting without withdrawal symptoms to be aggressive than patients presenting with alcohol withdrawal (p<.000, as shown in Table 1), with 68 patients not presenting aggressive behavior compared to 3 who were aggressive.
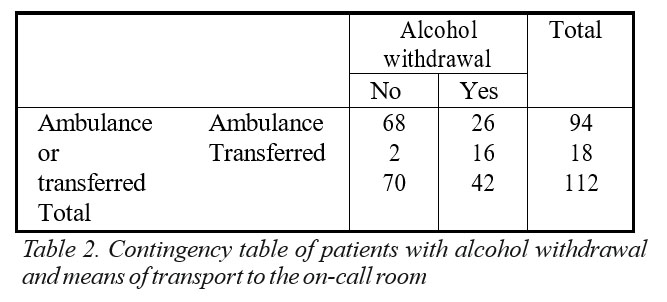
Transferred patients had remained admitted a longer period (Mdn=11.50) compared to patients who were brought by ambulance (Mdn=8.00, p=.027, r=.206). There was a significant association (Table 2) between the presence of withdrawal syndrome and the admission procedure (transferred versus not transferred), transferred patients were 21.05 times more likely to present with withdrawal symptoms compared to patients brought by ambulance (not transferred). There were 16 transferred patients who presented with alcohol withdrawal and 2 patients transferred in absence of this diagnosis.
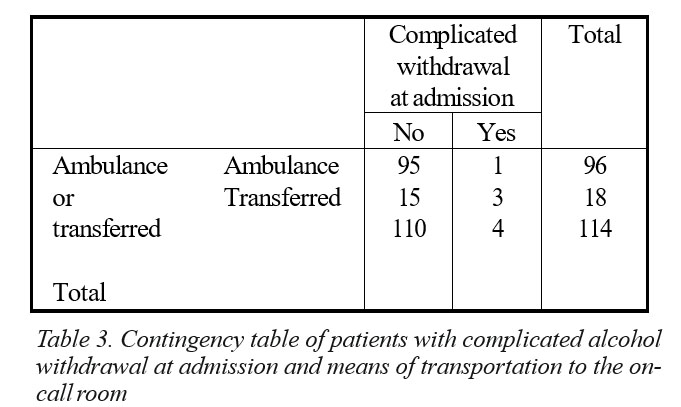
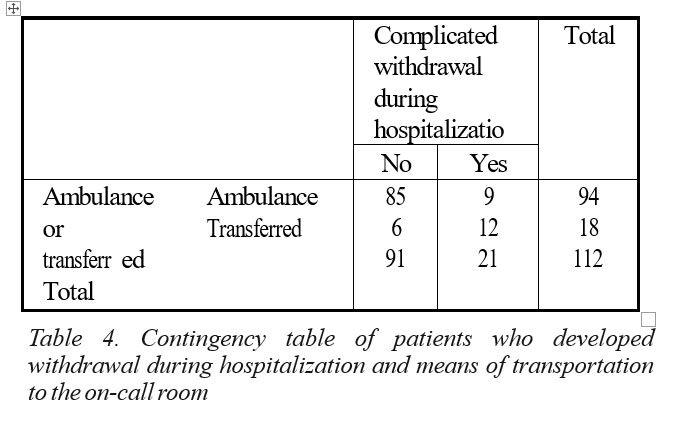
There was a significant association between the way patients were brought by and the presence of complicated withdrawal at admission. It was 20 times more likely that transferred patients to present with complicated withdrawal compared to those brought by ambulance (p=.012, Table 3). There was also 19.04 times more likely that patients admitted through transfer to develop complicated withdrawal while hospitalized compared with patients brought by ambulance (Table 4).
DISCUSSION
Out of all the discharges over a period of a year, 12.57% of patients had been diagnosed with an alcohol related disorder, making this diagnostic quite frequent in our hospital. Complicated withdrawal represents a third of the total patients diagnosed with alcohol withdrawal which brings forward on one side the difficulties of treating these patients and on the other side the need for a pattern to predict the development of complicated withdrawal.
There was a very large number (n=265, 81.79%) of patients admitted with complicated withdrawal that was transferred from other hospitals. In addition it was more likely that transferred patients develop complicated withdrawal. Alcohol withdrawal is a medical emergency for which psychiatric hospitals are often not prepared, making re-transfer procedures mandatory when complications develop. In addition, literature states a series of life-threatening complications (7-9) which are difficult to treat in a hospital with neither the specialists n o r t h e e q u i p m e n t n e c e s s a r y t o h a n d l e s u c h complications, in accordance with our observation that transferred patients and patients with alcohol withdrawal were admitted for a longer period. These data call for a close collaboration with other medical specialties, especially for these very difficult to treat patients.
Having alcohol dependence as a secondary diagnosis raises the number of hospitalization days. There is insufficient data to state whether the dependence itself causes the frequent readmissions or if alcohol dependence is a decompensating factor of the primary diagnosis or both the above are true.
Patients presenting with alcohol withdrawal were more likely to be insured than patients presenting with complicated withdrawal. This could be tied to the lack of employment in patients diagnosed with alcohol related psychiatric disorders.
Patients presenting without withdrawal had a higher chance of displaying aggressive behaviour compared to patients diagnosed with alcohol withdrawal which explains the physical and somatic burden of the withdrawal symptoms.
Due to the heterogeneity of our database more studies are needed to accurately describe which of these social and administrative factors predict complications of an alcohol withdrawal disorder and what measure must be implemented in order to manage alcohol induced disorders more efficiently.
CONCLUSION
Alcohol related disorders are common in our hospital. One of the most difficult entity to deal with is complicated alcohol withdrawal because of the high risk of mortality secondary to physical complications. The cost of managing such cases is rather high because patients often need consults from other specialists, non-voluntary admittance and transportation by ambulance and police squads. Most of the patients were not medically insured nor employed.
What is more, alcohol related disorders either as a primary or secondary diagnosis increase the number of days spent in the hospital. In these cases, primary prevention is not to be overseen and it is of great importance that we streamline the approach of alcohol related disorders.
ABBREVIATIONS
Mdn – median.
r – The correlation coefficient which measures the strength and direction of a linear relationship between two variables.
REFERENCES
1.Motoi Hayashida, M.D., Sc.D,Arthur I. Alterman, Ph.D., A. Thomas McLellan, Ph.D et al. Comparative Effectiveness and Costs of Inpatient and Outpatient Detoxification of Patients with Mild-to-Moderate Alcohol Withdrawal Syndrome. N Engl J Med 1989; 320:358-365.
2 . M a r i a B o n e a , M ă d ă l i n a C N e a c ș u , I o a n a V M i c l u ț i a . COMORBIDITIES OF ALCOHOL USE DISORDER. Romanian Journal of Psychiatry, vol. XX, No.2, 2018.
3 . h t t p : / / w w w . w h o . i n t / s u b s t a n c e _ a b u s e / publications/global_alcohol_report/profiles/rou.pdf?ua=1
4.American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
5.Elisaf M, Liberopoulos E, Bairaktari E, Siamopoulos K. Hypokalaemia in alcoholic patients. Drug Alcohol Rev 2002; 21:73.
6.Wadstein J, Skude G. Does hypokalaemia precede delirium tremens?
Lancet 1978; 2:549.
7.Schuckit MA, Tipp JE, Reich T, et al. The histories of withdrawal convulsions and delirium tremens in 1648 alcohol dependent subjects. Addiction 1995; 90:1335.
8.Elisaf M, Liberopoulos E, Bairaktari E, Siamopoulos K. Hypokalaemia in alcoholic patients. Drug Alcohol Rev 2002; 21:73.
9.Wadstein J, Skude G. Does hypokalaemia precede delirium tremens? Lancet 1978; 2:549.
10.Victor M. The role of hypomagnesemia and respiratory alkalosis in the genesis of alcohol-withdrawal symptoms. Ann N Y Acad Sci 1973; 215:235.
***