FACTORS ASSOCIATED WITH MEDICATION ADHERENCE IN PATIENTS WITH SCHIZOPHRENIA
Abstract
Introducere: Tratamentul schizofreniei necesită medicație administrată regulat pe termen lung. Non-aderența la medicația antipsihotică este considerată principalul motiv pentru reinternările in spital. Obiective: Evaluarea ratei de non-aderenţă la tratamentul cu antipsihotice la pacienţii cu schizofrenie, identificarea factorilor socio-demografici şi clinici care ar putea influenţa aderenţa la tratament. Metodă: Studiul a fost efectuat pe 60 de pacienţi, între octombrie 2014 şi octombrie 2016, aflaţi în evidenţă la diverse cabinete medicale de psihiatrie private din Timișoara, diagnosticaţi cu schizofrenie paranoidă (conform criteriilor ICD-10) și monitorizați timp de 6 luni în ceea ce priveşte aderenţa la tratamentul cu antipsihotice. La evaluarea iniţială au fost colectate date clinice privind pacienții și au fost aplicate scalele BPRS – Brief Psychiatric Rating Scale (pentru aprecierea intensității simptomatologiei psihiatrice) și ROMI – Rating of Medical Influences (utilizată pentru evaluarea atitudinii pacienților față de aderența la terapie). Scala BPRS a fost aplicată ulterior și pe parcursul monitorizării (o dată pe lună). În funcție de aderență, pacienții au fost împărțiți în două loturi, analizate comparativ. Rezultate: La nivelul întregului lot, durata medie a bolii a fost de 12.6 ± 7.6 ani, iar numărul mediu de spitalizări 6.4 ± 4.5. Aderența la tratament a fost mai bună la pacienții tineri. Pacienții necăsătoriți și cei trăind singuri au fost mai frecvent neaderenți. Am obținut diferențe semnificative între cele două loturi (aderenți vs. neaderenți) privind durata bolii (p=0.04) și durata medie a spitalizării (p=0.02). Principalele motive pentru non-aderență au fost disconfortul cauzat de efectele adverse ale medicației (37.5%) și faptul că tratamentul nu mai este necesar – din punctul de vedere al pacientului (21.8%). Cele mai importante motive pentru aderența la terapie au fost considerate: beneficiul zilnic adus de către medicația antipsihotică (32.1%) și prevenirea recăderilor (17.9%). Concluzii: Vârsta, statutul marital și durata bolii sunt factori care influențează aderența pacienților la tratament.
INTRODUCTION
From the perspective of any disorder with a significant degree of chronicisation, including schizophrenia, ensuring patient adherence to medical treatment starting from the first episode of the illness is essential. The treatment’s main objective for patients with schizophrenia is full control of symptoms with minimal impact on functioning, thus ensuring optimal quality of life. The chronic evolution of the disorder translates into the fact that most patients require antipsychotic medication for long periods of time, sometimes life-long, in order to achieve good control of symptoms and to prevent the recurrence of acute psychotic episodes and progressive cognitive impairment that are associated with t h e m ( 1 , 2 ) . T h e r e f o r e , c o n s t a n t a d h e r e n c e t o antipsychotic treatment is a major determinant for a favorable outcome. Unfortunately, a significant proportion of patients do not adhere to therapeutic indications. Treatment non-adherence rates in patients with schizophrenia cited in the literature varies, depending on the authors and the definition itself: between 20% and 89% (3) with an average of 49% of cases (4). The most significant consequences of antipsychotic treatment discontinuation are: increased number of relapses and hospitalizations, increased severity of symptoms during relapse, worsening of residual symptoms, substance abuse, and increased social cost (5,6,7). Although factors which influence adherence frequently overlap or influence each other, it’s still possible to distinguish factors related to: the patient (psychopathology, cognitive impairment, age, gender, personality traits, absence of insight, cultural beliefs regarding illness and health), treatment (tolerance, duration of treatment, onset of action and efficacy, unrealistic expectations in terms of benefit / risk ratio, delayed therapeutic effect and early side effects, subjective discomfort caused by the side effects), environmental (social environmental attitude towards the psychiatric treatment, availability of the family to support, assist and supervise the treatment, social support, stigma, financial situation), therapist-related factors (patient- psychiatrist relationship, therapeutic alliance, informing the patient about the disorder and treatment, perceived interest regarding the therapist’s interest towards the patient’s problems) (8,9,10). Adherence to treatment in schizophrenia is also affected by the duration and the consequences of discontinuing the medication: the consequences of non-adherence are mitigated by the insidious manner in which symptoms develop after treatment is discontinued so that the relationship between cause and effect becomes sometimes blurred both for patients and family, which can lead to maintaining non- adherent behavior. Although this grouping of factors is somewhat artificial, it can help the clinician to detect the various reasons for which the patient has developed non- adherence issues and to intervene accordingly.
The aim of the study was to assess the rate of non- adherence to antipsychotic treatment in outpatients with schizophrenia, to identify socio-demographic and clinical factors that may influence adherence to treatment and to record the reasons given by the patients as to why adherent or non-adherent behavior occurred.
MATERIALS AND METHODS
The study involved 60 patients diagnosed with schizophrenia from various psychiatric private practices located in Timișoara, Romania from October 2014 to October 2016. Inclusion criteria in the study were age between 18 and 65 years, the International Classification of Diseases 10 (ICD-10) diagnosis of paranoid schizophrenia, and the prescription of at least one antipsychotic agent. Cases of abuse or addiction to alcohol or drugs and those with limited capacity to give valid consent were excluded from the study. All patients used conventional or atypical antipsychotics and the method of administration was oral. Upon study entry, patients gave their informed consent and the research was approved by the local ethics committee. The study was conducted according to the principles stated in the Helsinki Declaration and the authors received no funding from any source.
Demographic and clinical characteristics of the patients (gender, age, marital status, educational status, professional status, the clinical form of schizophrenia, the duration of illness, number of hospitalizations, and antipsychotics used) were recorded. Data was obtained from the medical records supplied by the clinician and from the patients during the interview.
The term “adherence” was defined as the degree to which individuals follow directions for taking prescribed medication. Medication adherence was assessed through physicians` subjective perception, by direct questioning the patient or by questioning a family member. Adherence was assessed monthly by using the report given by a family member designated as responsible for this task. Non-adherence was defined as taking less than 75% of the prescribed dose within the preceding 30 days (adapted from Buchanan et al.,1992) (11).
At baseline, positive and negative symptoms and severity of hallucinations and thought disorder (conceptual disorganization) were quantified using BPRS (Brief Psychiatric Rating Scale) – the extended version, with 24 items (12).
An abbreviated version of the Rating of Medication Influences (ROMI) Scale was used to assess the attitudinal and behavioral factors that influence medication adherence (13). The ROMI Scale is a self- assessment scale which has two parts, the first part being semi-structured and includes questions about the patient’s lifestyle, treatment, patient and family attitudes towards treatment, active/passive adherence. The second part of the scale is divided into two sections, comprising the main reasons for adherence or non-adherence. This study used the second part of the ROMI Scale.
After clinical interview, the BPRS Scale and the ROMI Scale were applied at baseline. We divided the patients into two groups (adherent and non-adherent to treatment), that were assessed comparatively. The BPRS was used in the follow-up visits (on a monthly basis).
Data were analyzed using IBM SPSS Statistics for Windows (version 20). Statistical data processing calculated the statistic descriptive indicators, frequency, mean and standard deviation for numerical data. Because of the relative small sample size, a normality test was applied (the Shapiro-Wilk normality test). The test revealed a non-gaussian data distribution and therefore, to compare groups, we used a non-parametrical test (the Mann-Whitney U test). For comparing categorical data, we utilized the χ² test. The level of significance was set at 0.05. All results were two-tailed.
RESULTS
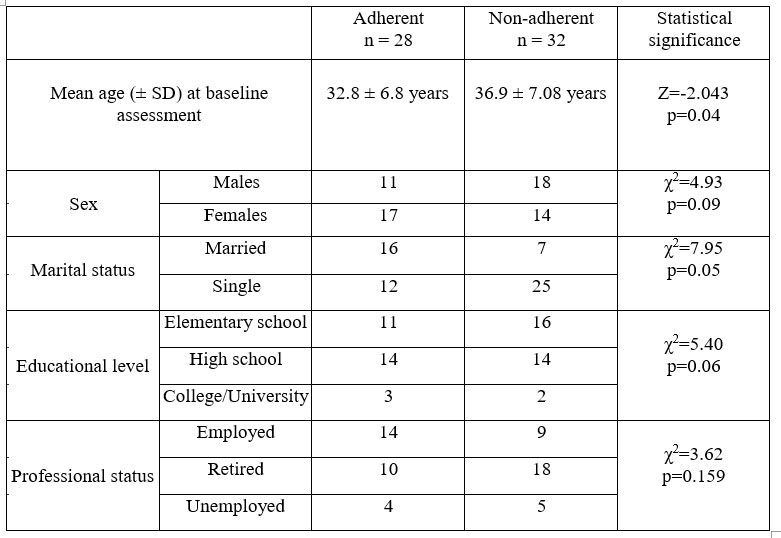
Baseline characteristics of the patients are presented in Table 1.
Thirty-one were female (51.7%) and twenty- nine (48.3%) male and their mean age was 36 years (SD=11.4). Out of the 60 patients, 23 (38.3%) were married, 37 (61.7%) were single (not married, separated or divorced). Upon entry into the study 23 patients (38.3%) were employed, 28 (46.7%) were retired and 9 of them (15%) were unemployed. In terms of educational level 27 of them (45%) had completed elementary school, 28 (46.7%) were high school graduates and 5 (8.3%) college or university graduates.
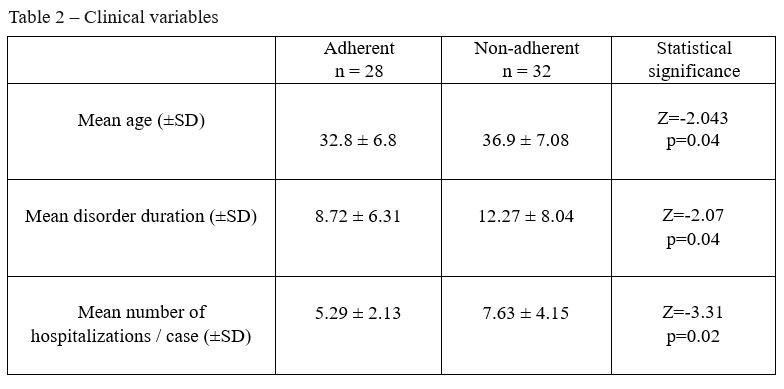
We noted statistically significant differences between groups considering mean age, the duration of the illness and mean number of hospitalizations, as can be observed in Table 2.
We noticed that younger patients were more adherent to treatment than elderly patients, whilst non- adherent were significantly more frequent single patients (χ²=2.315, p=0.05) and those living alone (χ²=3.115, p=0.002). We found no significant statistical associations between adherence and educational level (χ²=0.21, p=0.156), between adherence and professional status (χ²=0.159, p=0.23), or between adherence and gender (χ²=0.135, p=0.38).
The mean BPRS values obtained in the evaluations show a mild severity of symptomatology, which was maintained relatively constant during the study in both groups of patients. The difference between the groups during the direct evaluation regarding increased symptom severity in the non-adherent group was not validated from a statistical point of view (Table 3).
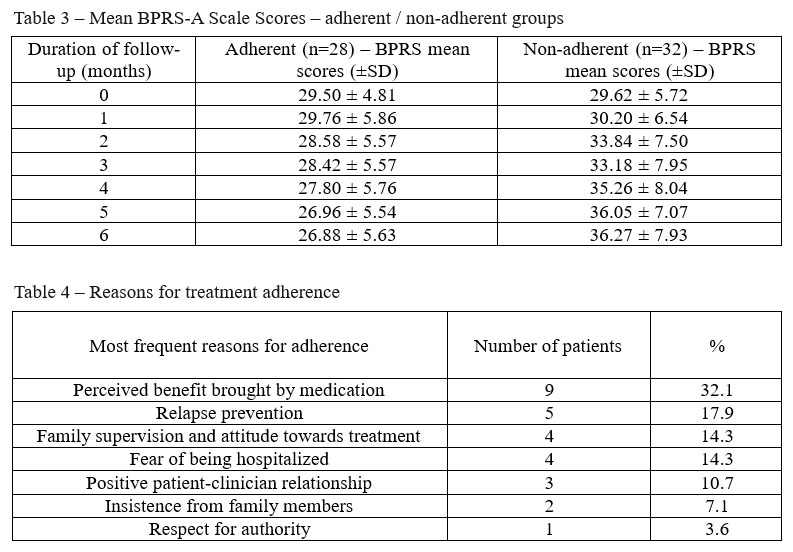
Another aspect studied was the patient’s motivation towards medication adherence or non- adherence. The most important reasons for adherence, after ROMI Scale were: the perceived daily benefit brought on by antipsychotic medication (increased quality of sleep, decreased anxiety levels, diminished hallucination frequency and intensity, increased control over their thoughts), relapse prevention, positive family beliefs and supervision, fear of being hospitalized and a positive patient-clinician relationship (Table 4).
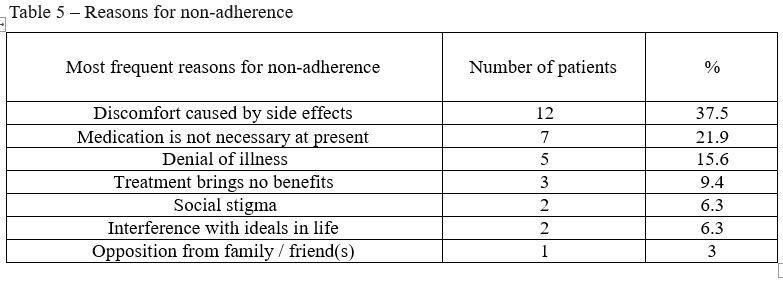
The most important reasons for non-adherence were discomfort caused by the adverse effects of the medication (extrapyramidal and anticholinergic effects, weight gain), followed by “medication is not currently needed” – from the patient’s perspective, denial of illness, treatment without benefit, social stigma and interference with ideals in life, opposition from family. Data are presented in Table 5.
DISCUSSIONS
The study investigated reported non-adherent forms of behavior and their detection by clinicians in patients with paranoid schizophrenia. Before discussing the findings in detail, it is important to comment on the use of self-report measures of adherence. No method of adherence assessment is perfect, but the specificity of self- report is considered to be comparable with plasma measurements and event monitoring techniques (14). Stephenson (15) suggests that the sensitivity of self-report is less reliable but is a simple and low-burden measure that can be applied to a large sample of patients. The rate of non-adherence found in our sample over a 6-month period (53.30 %) is in agreement with those found in the literature – approximately 50% (11,15,16,17). Socio-demographic characteristics did not differ much between patients who had good adherence and those who were non-adherent. The non-adherent group had a higher mean age at the baseline assessment than those in the adherent group. Literature is equivocal in terms of age, some studies finding more often non-adherent behavior in young age groups (10,18), other report adherence problems in older people (19,20). Possible explanations are the tendency to be non-conformant, thus refusing to follow a rigorous, planned schedule for the young and in the case of older people the potential presence of memory disorders and concomitant medication for various somatic disorders that may contribute to lower adherence (21,22). A significant correlation was found regarding non-adherent behavior and the marital status. Single patients and especially the ones who lived alone were more likely to be non-adherent. The correlation found between illness duration and non- adherent behavior is in concordance with the literature data, supporting the idea that risk for non-adherence increases in parallel with the disorder duration, and acknowledged as being present in other chronic psychiatric or non-psychiatric disorders (23,24). The mean number of hospitalizations/ non-adherent case suggests the role of risk factors for relapses and consequently a more unfavorable development which can occur because of non-adherence to treatment. A significant difference regarding symptom severity between adherent and non-adherent patients was not found in our study. The severity of the disorder has been found by many authors to correlate with adherence, which is understandable since patients presenting more severe psychopathology would be expected to be less adherent to treatment. On the other hand, it’s known that non- adherence to treatment is determined by multiple factors, including the severity of symptoms but this is not considered a unique and necessary cause (11,25). The main motivation for adherence was the perception of a potential benefit. Patients need to feel better, regarding something that disturbed them (example: sleep disturbance, anxiety, hallucinations). The perception of benefit and a subjective perception of well-being seem to have been more consistently correlated with adherence (26). Supervising the intake of medication by family or friends and positive attitudes towards medication was frequent in the adherent patients. A positive relationship with the clinician was quoted by only 10.71% of patients as a reason for adherence. In other studies, this reason is more frequently cited (27) than in our study. The clinician- patient relationship is however difficult to assess in terms of methodology. It is widely recognized that a good therapeutic alliance can influence patient attitude towards the disorder and treatment. The information the clinician provides his patients with, regarding the disorder, about the effects and usefulness of treatment, also about their side effects, can significantly contribute to improving adherence. The most common reason quoted by non- a d h e r e n t p a t i e n t s w a s t h e a d v e r s e e ff e c t s o f antipsychotics. Side effects, particularly extrapyramidal and anticholinergic effects are the source of considerable distress, they have a stigmatizing role and potentially unpleasant consequences, decreasing the patient’s quality of life as well as his desire to take antipsychotic medication ever again. The next reason quoted by the patients was that medication is not necessary now, reflecting the response of patients on disease knowledge and beliefs. It is obvious that if the patient feels well and believes that schizophrenia is an unimportant disorder that doesn’t require continuous treatment, adherence will be compromised.
CONCLUSIONS
In the present study, we found a high rate of non- adherence during the 6-month follow-up of outpatients with schizophrenia. Non-adherent behavior was more frequently found in the elderly and in those living alone. D i s o r d e r d u r a t i o n a n d t h e m e a n n u m b e r o f hospitalizations per case were higher in the non-adherent group, the second variable suggesting the role of risk factor for relapse that non-adherence to treatment represents. In the opinion of the assessed patients, the most important reason for adherence was the perception of the daily benefit brought by the medication and for non- adherence the discomfort caused by the side effects of the antipsychotics. Identifying and understanding the reasons for non-adherence to treatment represents a strategy of improving the patient’s commitment in long-term therapy. The results suggest that outpatients with schizophrenia
who have various reasons for non-adherence are associated with actual non-adherence and the ROMI Scale may be useful for predicting such behavior. Improved treatment adherence in schizophrenia can reduce the risk of relapse and its morbid consequences and perhaps promote higher functioning through better therapeutic engagement.
LIMITATIONS
Our study must be interpreted in light of some limitations: the relatively small patient samples, adherence wasn’t studied according to antipsychotic classes, which could have (potentially) influenced the end results. Like other studies of medication adherence among individuals with psychotic disorders, the present study was hampered by inherent selection biases, because individuals who consent to participate in such research and complete the required assessment are likely to be more compliant in taking medication.
AKNOWLEDGEMENTS
All authors have contributed equally to the present study and approved its final version.
DISCLOSURES
The authors have no conflict of interest to disclose for the present article.
LIST OF ABREVIATIONS
BPRS: Brief Psychiatric Rating Scale
ROMI: Rating of Medication Influences
Table 1 – Socio-demographic data – adherent / non-adherent group
REFERENCES
1.Lieberman JA, Tollefson GD, Charles C et al. Antipsychotic Drugs Effects on brain morphology in first episode psychosis. Arch. General Psychiatry 2005; 62: 361-70.
2.McCabe R, Bullenkamp J, Hansson L et al. The therapeutic relationship and adherence to antipsychotic medication in schizophrenia. PLoS One 2012; 7(4):1–5
3.Knapp M, King D, Pugner K. Non-adherence to antipsychotic medication regimens Associations with resource use and costs. Br J Psychiatry 2004; 184: 509-16.
4.Naber D, Karow A, Lambert M. Subjective well-being under neuroleptic treatment and its relevance for compliance. Acta Psychiatrica Scandinavica 2005; 111(427): 29-34.
5.Christy LM Hui, Eric YH, Chen CS et al. Detection of non-adherent behavior in early psychosis. Australian and New Zealand Journal of Psychiatry 2006; 40: 446-451.
6.DiBonventura M, Gabriel S, Dupclay L, Gupta S, Kim E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry 2012; 12:20.
7.Nicolino PS, Vedana KG, Miasso AI, Cardoso L, Galera SA. Schizophrenia: adherence to treatment and beliefs about the disorder and the drug treatment. Rev Esc Enferm USP 2011; 45(3):708-15.
8.Woerner MG, Mannuzza S, Kane JM. Anchoring the BPRS: an aid to improve reliability. Psychopharmacol Bull 1988; 24 (1): 112-17.
9.Novick D, Haro JM, Hong J et al. Regional differences in treatment response and three year course of schizophrenia across the world. J Psychiatr Res 2012; 46:856–864.
10.Lee H, Kane I, Sereika SM, Cho RI, Jolley CJ. Medication-taking behaviours in young adults with schizophrenia: a pilot study. J Psychiatr Ment Health Nurs 2011; 18:418–424.
11.Buchanan A. A Two Year Prospective Study of Patients with treatment compliance in schizophrenia. Psychol Med 1992; 22 (3): 787-97.
12.Lukoff D, Nuechterlein KH, Ventura J. Manual for the Expanded BPRS. Schizophrenia Bull 1986; 12:584-602.
13.Waiden P, Rapkin B, Mott T. Rating of medication Influences (ROMA Scale) in schizophrenia. Schizophr Bull 1994; 20: 297-310.
14.Byerly M, Fisher R, Whateley C et al. A comparison of electronic monitoring vs. clinician rating of antipsychotic adherence’s in
Outpatients with schizophrenia. Psychiatry Research 2005; 28: 129-33.
15.Stephenson BJ, Rowe BH, Haynes RB et al. Is this patient taking the treatment as prescribed? JAMA 1993; 269: 2779-81.
16.Adams J, Scott J. Predicting medication adherence in severe mental disorders. Acta Psyh Scan 2000; 101: 119-24.
17.Dolder CR, Lacro JP, Dunn LB et al. Antipsychotic medication adherence: There is a difference between typical and atypical agents. American Journal of Psychiatry 2002; 159: 103-12.
18.Hudson TJ, Owen RR, CR Trush et al. A Pilot Study of barriers to medication adherence in schizophrenia. J Clin Psychiatry 2004; 65 (2): 211-16.
19.Fleischnacker WW, Oehl MA, Humera M. Factors influencing compliance in schizophrenia patients. J Clin Psychiatry 2003; 64 (16):
10-13.
20.Ritchie CW, Harrigan S, Mastwyk M et al. Predictors of adherence to atypical antipsychotics (risperidone or olanzapine) in older Patients with schizophrenia: an open-Study of 3 (1 / 2) Years duration. Int. J. Geriatrics. Psychiatry 2010; 25: 411-18.
21.Kim SW, Shin IS, Kim JM et al. Association between attitude towards medication and neurocognitive function in schizophrenia.
Clin Neuropharmacol 2006; 29: 197-205.
22.Kane JM, Kishimoto T, Correll CU. Non‐adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry 2013; 12(3): 216-226.
23.Gallego JA, Nielsen J, De Hert M, Kane JM, Correll CU. Safety and tolerability of antipsychotic polypharmacy.
Expert Opin Drug Saf 2012;
11:527–542.
24.Perkins DO. Predictors of noncompliance in Patients with Schizophrenia. J Clin Psychiatry 2002; 63: 1121-1128.
25.Kwon J, Collins A, Christenson B. Medication compliance in patients with schizophrenia taking oral antipsychotics. International Journal of Psychopharmacology 2000; 3(1): 124-125.
26.Fenton WAS, Bleuer CR, CR Heinssen. Determinants of medication compliance in schizophrenia: empirical and clinical Study. Schizophr Bull 1997; 23: 637-51.
27.Bennasar MR, Planas M. Compliance in schizophrenia. Advances in Schizophrenia and Clinical Psychiatry 2004; 1(3): 78-84.
***