TRENDS IN CHILD AND ADOLESCENT PSYCHIATRIC DIAGNOSES IN A ROMANIAN INPATIENT UNIT BETWEEN 1990 AND 2014
Abstract
Objective. This paper aims to describe trends in diagnostic data in discharged patients from a regional child and adolescent psychiatric inpatient unit in Romania, over a 25-year period (1990-2014). Method. Data on discharge diagnosis of the 30854 patients from the study timeframe were analyzed. Diagnostic formulations in the years prior to ICD implementation were converted into ICD-10 specific disorders/ class of disorders. Results. Results showed a significant increase in proportion of autism spectrum disorders and hyperkinetic disorders over time and a significant decrease of stress related, dissociative and somatoform disorders. The number of psychotic disorders was constant over time, mood disorders had peak frequencies in 2003 and 2014 and anxiety disorders has a twofold increase from 2007 to 2014. Conclusions. This study demonstrates a major shift in the patterns of mental health disorders diagnosed among children and adolescents at our clinic over the last 25 years. Defining the current mental health needs of young people and adjusting service delivery in child and adolescent psychiatric settings have become of great importance in recent years.
According to the U.S. National Institute of Mental Health, over 20 percent (1 in 5) children, either currently or at some point during their life, have had a seriously debilitating mental disorder and about 13 percent of children ages 8 to 15 had a diagnosable mental disorder within the previous year (1). World Health Organization states that mental health disorders in children and adolescents are of great concern because of their high prevalence and the accompanying disabilities (2).
The Centaur project was the only systematic epidemiologic survey of child and adolescent psychiatric disorders conducted in Romania between 1981 and 1984, on a nationwide sample of 14812 subjects aged 10 months to 16 years. The study reported an overall point prevalence of 11.7% for any psychiatric disorder in children and adolescents and also assessed the individual prevalence of 90 psychiatric and neurological disorders, based on DSM- III and ICD-9 criteria (3). More recent, population-based representative data are not available in Romania, at this moment.
This paper aims to describe trends in diagnostic data of patients discharged from a regional child and adolescent psychiatric inpatient unit in Romania, over a
25-year period (1990-2014).
METHOD Setting
The present study was conducted in the Department of Child and Adolescent Psychiatry of the “Prof. Dr. Alexandru Obregia” Psychiatry Clinical
Hospital in Bucharest, Romania. The clinic is one of three university clinics of Child and Adolescent Psychiatry in the country and the largest one, with a total of 70 beds at present. The clinic functions as an inpatient unit for acute patients, who are admitted for continuous hospitalization or day hospitalization. The patients addressing the clinic are both inhabitants of the city of Bucharest (approximately 2103000 inhabitants) and the neighboring districts.
An important legislative change in this field, with consequences for the organization of the clinic took place in Romania in 1996, when the specialty called Infantile Neuropsychiatry was officially divided into two distinct medical specialties, Paediatric Psychiatry (Child and Adolescent Psychiatry) and Paediatric Neurology. The actual transition within the hospital with the full separation of psychiatric from neurological cases into two different departments took place gradually, until the year 2000. Thus, prior to this period, patients addressed the clinic either for a neurological or for a psychiatric issue, and only later on did the pathology become almost exclusively of a psychiatric nature. The neurological cases were excluded from the analysis performed in this study.
Procedure and analysis
Data of of 39562 patients hospitalized in the clinic between 1990-2014 have been initially collected in the present study. Of these patients, 8708 were exclusively neurological cases and were therefore later removed from the analysis. Ultimately, 30854 patients with psychiatric pathology, aged between 1 and 18, admitted as continuous hospitalization inpatients, were included in the study.
In 2009, the hospital introduced a computerized system for the manipulation and storage of patient information. Data for the patients who had been hospitalized before 2008 existed only on paper, in the clinical observation sheets and patient registers. Thus, an electronic database was initially created by the transcription of patient data (age, gender, city, diagnoses upon discharge) for the patients who were admitted between 1990 and 2009. Clinical data of the patients who were admitted between the years 2012 and 2014 were provided by the Department of Medical Statistics within the hospital, through export from the computerized system of the hospital (Medical CM).
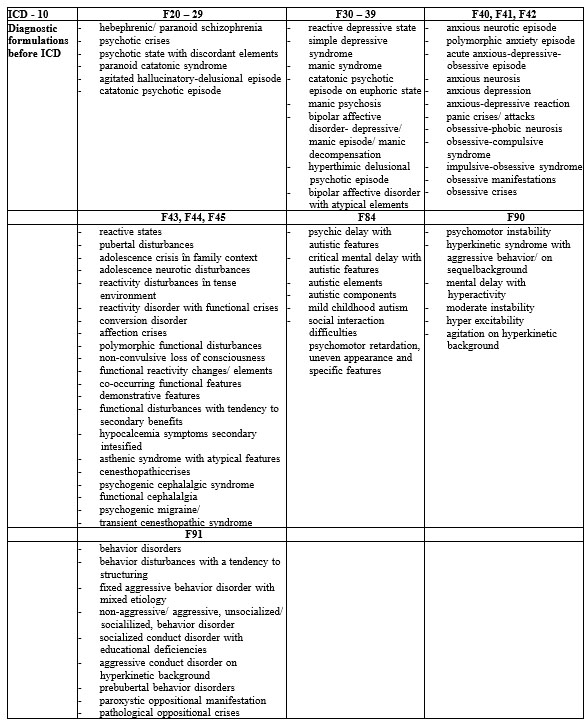
Table 1 Diagnostic formulations prior to the implementation of ICD
For logistical reasons, data on admissions from the second half of 2009 and the years 2010 and 2011 could not be accessed and were therefore not included in the present study.
For the study of the evolution of pathology within the clinic, all the diagnoses upon discharge of the 30854 patients from the study period were introduced in the analysis. Since 2008, all diagnoses are coded using the ICD-10 (International Classification of Diseases) codes, due to the introduction of the DRG (Diagnostic-related group) in the hospital. Before 2008 however, due to the absence of a standardized taxonomic system of diseases, the diagnoses were highly flexible, lengthy, with influences derived from French and Russian schools of psychiatry and dependent on each doctor’s experience and training. Moreover, the medical language used was often different from one doctor to another. Therefore, a major step prior to the analysis was to translate these diagnoses into the closest possible ICD diagnostic categories, by a team of professionals within the clinic. This process was a difficult one, and due to the fact that, in many cases, a specific ICD code for a certain diagnosis was not identified, for certain pathologies, the preferred method was to determine the diagnostic category only (e.g. for any mood disorder the F30-F39-mood (affective) disorders ICD-10 code was used).
Thus, the analysis of the evolution of the pathology within the clinic between 1990 and 2014 was focused on the following disorders or diagnostic classes: F20-29 (schizophrenia, schizotypal and delusional disorders); F30-30 (mood disorders); F40,F41 and F42 (anxiety disorders and OCD); F43, F44 and F45 (stress related, dissociative and somatoform disorders); F84 (pervasive developmental disorders –currently referred to as autism spectrum disorders); F90 (hyperkinetic disorders); F91 (conduct disorders). Table 1 contains relevant examples of diagnostic formulations the years preceding the introduction of ICD in the clinic.
Due to the difference in the total number of discharges with a psychiatric diagnosis per year (ranging from 852 in 1993 and 2567 in 2013), we defined the frequency of disorders using percentages instead of absolute values. Least-squares regression has been used to determine time trends in rates of disorders.
RESULTS
Table 2 displays the frequencies (in percentages) of the mental disorders in the clinic, for each of the years included in the analysis. For each year, the reported percentage represents the number of diagnoses upon discharge of a certain disorder out of the total number of patients with a psychiatric diagnosis admitted to the clinic that year.
Regarding psychotic disorders in the F20-F29 category (schizophrenia, schizotypal and delusional disorders), no significant fluctuations are observed throughout the study period (F(1,21)= .75, p= .39)(Table 3), with a frequency of 2.3% to 7.6% of all cases per year (Figure 1a). Affective disorders (Figure 1b) experience an upward trend in the 1990-2003 time period (r2= .76, F(1,12)= 39.7, p= .000), from 3.9% in 1990 to 13.9% in 2003, equal to a 3.5-fold increase in frequency. During the following years affective disorders decreases in frequency, reaching 4.97% in 2009, with a subsequent increase after 2009 leading to a frequency of 10.3% in 2014.
Anxiety disorders (Figure 1c) have a minimum frequency of 2.8% in 1997 and 1998 and a maximum of 9.13% in 2014. The increase over the entire time period is a significant one (F(1,21)= 18.34, p= .000)(Table 3), with the largest increment observed between 2007 and 2014, when the proportion of anxiety disorder doubled. Regarding the stress related, dissociative and somatoform disorders a downward trend is observed, from a maximum of 23.6% in 1991, to 6.4% in 2013, translated into a four time reduction in the total number of cases over time (Figure 1d).
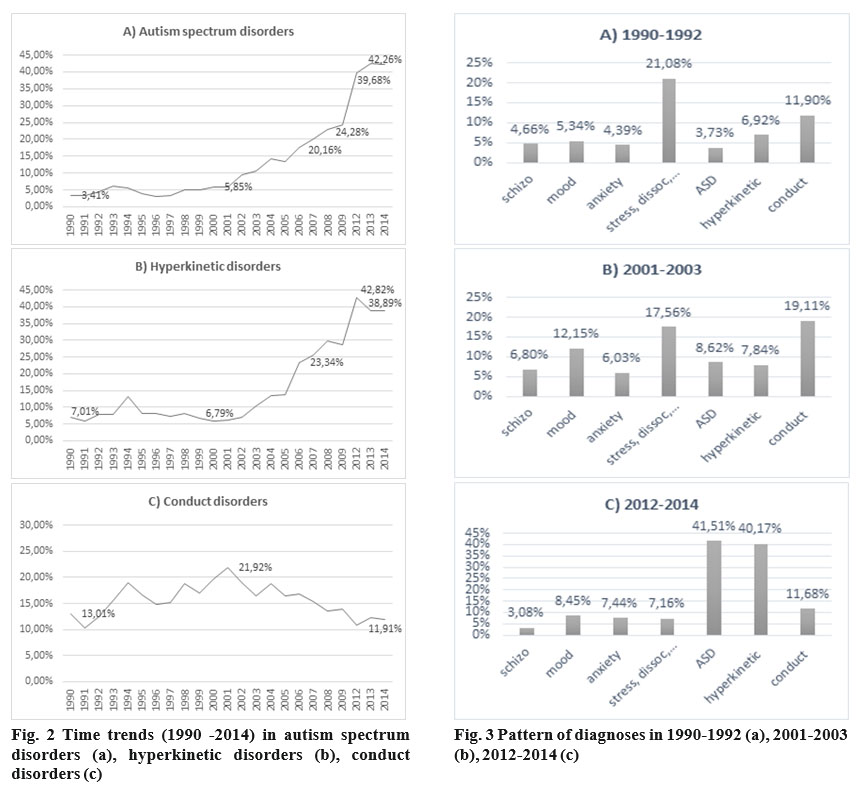
Autism spectrum disorders showed the highest increase during the 1990-2014 study period (r2= .80, F(1,21)= 86.2, p= .000)(Table 3). Thus, if in 1990 through to the year 2000 the frequency of ASD was 3-6% of the total number of cases admitted to the clinic in one year, the percentage grew to 17-22% in 2005 to 2007, only to reach 39-42% in 2012-2014 (Figure 2a). Therefore, the frequency of ASD in the clinic has increased 12-fold in 2014 when compared to 1990. The second largest increase in frequency during the study period was observed for hyperkinetic disorders (Figure 2b). Between 1990 and 2002 the frequency of the diagnosis was relatively stable, with a mean of 7.6%. Starting the following year, however, the frequency of hyperkineti disorders began to rise from 10.4% in 2003 to
25.6% in 2008 and it reached 38-42% in 2012-2014 with a peak in 2012. This increase is significant throughout the entire study period study and the observed trend is almost linear between 2002 and 2014 (r2= .93, F(1,9)= 129.7, p= .000)(Table 3). Almost half of all cases were co-morbid with autism spectrum disorders (18.1% out of 38.8% in 2014).
Conduct disorders register a rise in frequency in 1990-2001, from 13.0% in 1990 to 21.9% in 2001 (r2= .67, F(1,10)= 20.5, p= .000). After reaching a maximum in
2001, the number of diagnoses within the group of conduct disorders began to decrease, reaching 11.9% in 2004 (r2= .86, F(1,10)= 66.8, p= .000) (Figure 2c).
Estimates based on averaging 3 consecutive years’ data, at the beginning of the study period (1990- 1992), in the middle (2001-2003) and at the end (2012-
2014) reveals the following (Figure 3): the most common discharge diagnoses in 1990-1992 were stress-related, dissociative and somatoform disorders (21.1%), followed by conduct disorders (11.9%); in 2001-2003, conduct disorders reached a peak frequency, with a proportion of 19.1%, the number of stress related, dissociative and somatoform disorders start to decrease (17.6%) and mood disorders also reached their highest level through the entire study period (12.2%); between 2012 and 2014, autism spectrum disorders and hyperkinetic disorders show a significant increase, each of these attaining a proportion of 40% of all the cases, conduct disorders start to decrease, reaching a similar frequency to the one observed in 1990-2014 (11.6%) and the proportion of anxiety disorders rises to 7.4%
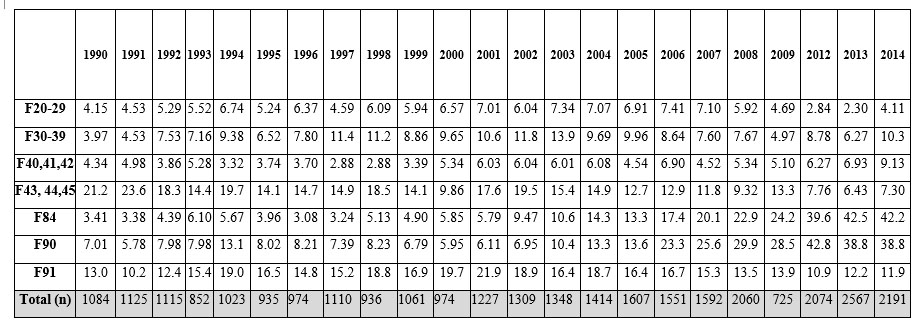
Tabel 2 Frequency (percentages) of mental disorders in the clinic between 1990 and 2014 F20-29schizophrenia, schizotypal and delusional disorders; F30-30 mood disorders; F40, F41, F42 anxiety disorders and OCD; F43, F44, F45 stress related, dissociative and somatoform disorders; F84 autism spectrum disorders; F90 hyperkinetic disorders F91 conduct disorders
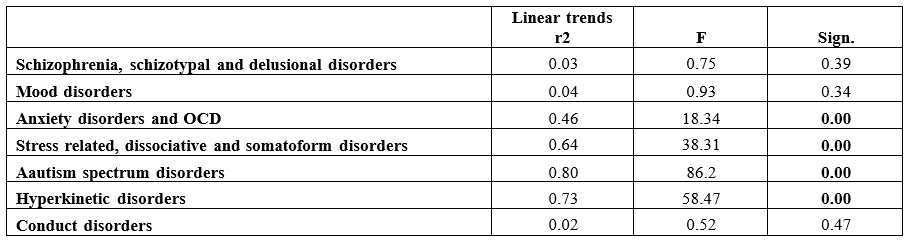
Tabel 3 Linear trends
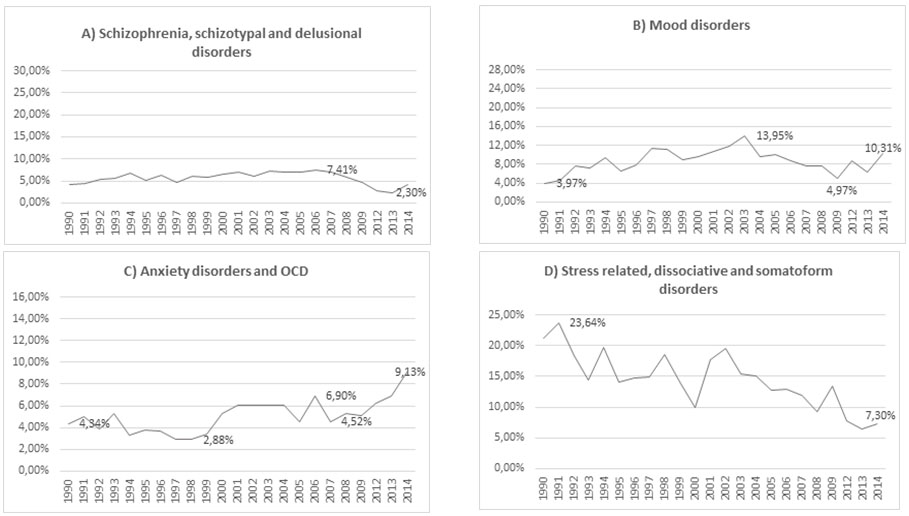
Fig. 1 Time trends (1990 -2014) in schizophrenia, schizotypal and delusional disorders (a), mood disorders (b), anxiety disorders and OCD (c), stress related, dissociative and somatoform disorders (d)
DISCUSSION
The present study demonstrates a major shift in the patterns of mental health disorders diagnosed among children and adolescents at our clinic over the last 25 years. Highlighting this change is of major significance, both for clinical practice and for the community. In clinical practice, this shift in pathology supports the need to optimize hospital facilities, including human resources (type and number of personnel, professional training), the assessment and monitoring tools and, last but not least, the therapeutic interventions. The results of this study also prove the need for the undertaking of epidemiological studies on general populations. Identifying and quantifying the current issues regarding the mental health of children and adolescents should lead to optimizing the specific mental health policies. This could be achieved through providing adequate training to professionals in the field, improving the welfare and educational systems and increasing the level of awareness among the general population (facilitating the addressability towards medical service providers and social mobilization).
One of the main results of this study is the overwhelming increase in the number of Autism spectrum disorders, diagnosed among the patients in our clinic over the years, from 3,4% ASD diagnoses upon discharge in 1990 to 42% in 2014, translated into a twelvefold increase in frequency. This increase may be largely explained by the actual increase in the prevalence of the disorder, as reported worldwide. The CDC, in their 2014 Morbidity and Mortality Monthly Report states that “The global prevalence of autism has increased twentyfold to thirtyfold since the earliest epidemiologic studies were conducted in the late 1960s and early 1970s.” CDC’s ADDM Network in 2014 reports that about 1 in 68 children (8 year-olds) has been identified with ASD (4). This new estimate is roughly 30% higher than the estimate for 2008 (1 in 88), roughly 60% higher than the estimate for 2006 (1 in 110), and about 120% higher than the estimates for 2002 and 2000 (1 in 150) (4). Another factor contributing to the high number of ASD patients in our clinic was the increase in addressability over the last years, due to the ASD awareness campaigns aimed for the general public. Other causative factors would be the reduced capacity of the outpatient network, both in the the actual number of professionals and the lack of specific assessment tools for ASD, as well as the mandatory yearly assessment of children suffering from ASD who benefit from disability allowance.
Another significant finding of this study was the rise in the number of diagnoses of attention deficit hyperactivity disorder, which began in 2003. Until 2003 the frequency of this diagnosis was relatively stable (at 7% per year). In 2008 however, almost 25% of the patients were diagnosed with ADHD and by 2014, this percentage rose to almost 40%. This trend could be partially explained by the increasing comorbidity of ADHD with ASD. Thus, in 2014, almost 45% of the ADHD diagnoses are found in children suffering from ASD. This result is consistent with the available studies in literature, which stipulate that 30% to 80% of ASD patients also suffer from ADHD (5-8). Moreover, there was also an increase in the rate of ADHD diagnosis in children without ASD, in the timeframe that was analyzed. This increase could be attributed to a greater knowledge of this disorder among professionals as well as an actual rise in the prevalence of ADHD in the general population. Up until the introduction and use of the DSM and the ICD diagnostic manuals in Romania, psychiatrists’ awareness regarding this pathology (often called „psycho-motor instability” in the 1990’s) was fairly low, and therefore the disorder often remained undiagnosed. Worldwide, the rate of ADHD prevalence among children aged 5 through 18 years, increased from 1.1% in 1990, to 2.8% by 1995 (9), reaching up to 5.29% in 2007 (10). In 2012, results of a meta-analysis on the prevalence of ADHD, generated estimates in children and adolescents, ranging from 5.9% to 7.1%, depending on the source of information for the diagnosis (11).
Another major shift in the pathology from our clinic was the significant decrease in the diagnostic classes related to stress, conversion and dissociative disorders. In the present analysis, these disorders have been combined into a single group, because diagnostic formulations prior to the introduction of ICD coding did not allow for a clear distinction between each of these disorders. Still, in the 90’s, diagnoses such as “functional disturbances / crises” or “reactivity disorder” accounted for approximately 20 % of all cases, compared to only 6-7% in 2012-2014. Knowledge regarding the epidemiology of these disorders among children and adolescents is limited, mainly because of variable case definitions, assessment instruments and study populations (12). The influences of the cultural environment, responsible for social learning, modelling and different ways of expressing distress play an important role in the development and course of these symptoms. It may be speculated that this form of expressing psychological distress may be more frequent in certain cultural environments, in individuals with lower socioeconomic status and lack of education, in individuals with a history of physical abuse or neglect in childhood. A study published in India in 1993 also found high rates for this pathology in children, of approximately 14% in outpatients and almost 30% among inpatients (13). Therefore, the high frequency of these disorders among patients in our clinic during the 90’s could be explained by the poor level of economic development in our country in that time period, by the almost exclusively eastern influences in our culture (after almost 50 years of living under a communist regime) and by the low level of significance attributed to the understanding and fulfillment of emotional needs in general, during those times.
The psychotic disorders category, including schizophrenia, schizotypal and delusional disorders registered a stable and relatively low frequency in our clinic, during 1990 through 2014. Worldwide, the onset of schizophrenia prior to the age of 13 is still considered rare, with an incidence lower than 1 in 10000 children (14), but up to 20% of adults with schizophrenia become ill before the age of 18 (15). Data regarding time trends in early onset schizophrenia are lacking.
Affective disorders have fluctuated in frequency during the studied time period in our clinic, with a minimum of 4% of all cases in 1990 and two peak frequencies in 2003 (13%) and 2014 (10%). The degree to which these rises in frequency are real or not may be verified through future epidemiological national studies. A meta-analysis published in 2006 in the UK regarding time trends in child and adolescent depression concludes:
„There is no evidence for an increased prevalence of child or adolescent depression over the past 30 years. Public perception of an ‘epidemic’ may arise from heightened awareness of a disorder that was long under-diagnosed by clinicians” (16). The prevalence rate of major depression in children and adolescents is estimated between 0.2% to 3.0% in the general population, and between 0.0% and 0.9% for bipolar disorders (17).
This study is characterized by a number of limitations that must be considered when interpreting the findings. First, the reliability of converting former diagnostic formulations into ICD-10 disorders does not ensure accuracy. Second, only a few types of information about the patients were recorded in hospital registries, thus limiting the analysis that could be performed. Finally, as data from only one clinical setting were utilized, the results should not be interpreted as nationally representative.
This study highlights the changing profile of mental disorders in inpatient care, demonstrating the need to reevaluate services delivered to children and adolescents. These findings also emphasize the need for future epidemiological research to improve the knowledge about the state of child mental health at the national level. As evidence suggests that lifetime mental disorders first appear before the age of 18 years, collaborative efforts must be brought to the forefront, prioritizing the care of children and adolescents.
Ethical standards
This study was approved and conducted according to the procedures of the ethics committee of “Prof. Dr. Alexandru Obregia” Psychiatry Hospital. Patient data were obtained with the permission of the local ethics committee with respecting the current laws regarding data protection. This is a register-based research, the manuscript does not contain clinical studies.
Acknowledgments
The authors thank for significant contribution in data collection to all their colleagues: Aiten Abzait, Cristian Adam, Iulia Badarau, Alexandra Buica, Diana Barbulescu, Paula Chicos, Iuliana Ciobanu, Ana Maria Ciuca, Malina Coman,Sabina Duta, Laura Gheorghica, Georgiana Grigore, Elena Iliescu, Hermina Ionescu, Cristian Luhovschi, Andra Magalu, Andra Melescan, Giorgiana Mihai, Mirela Militaru, Ioana Mocanu, Georgiana Murariu, Stefan Olteanu, Cristian Popa, Oana Rus, Raluca Soanca, Andra Soos, Mihaela Sprinceana, Alina Stan, Mihaela Stancu, Madalina Toma, Georgiana Tocaci, Iulia Turtoi, Ioana Viziteu
Conflict of interest
The authors declare that they have no conflict of interest.
References
1. National Institute of Mental Health. Any Disorder Among Children. http://www.nimh.nih.gov/health/statistics/prevalence/any-disorder- among-children.shtml Accessed 25 March 2016
2. The World Health Organization. Global burden of mental disorders and the need for a comprehensive, coordinated response from health and s o c i a l s e c t o r s a t t h e c o u n t r y l e v e l . 2 0 1 2 . http://apps.who.int/gb/ebwha/pdf_files/WHA65/A65_10-en.pdf?ua=1
Accessed 25 March 2016
3. Grigoroiu Serbanescu M, Christodorescu D, Cantilli L, Jost L, Nedelcu H. Epidemiology of child and adolescent psychiatric disorder in a Romanian nationwide sample. I. Age group prevalence. Rom J Neurol
1997; 37(I-2):85-94.
4. CDC. Prevalence of autism spectrum disorders. Autism and Developmental Disabilities Monitoring Network, United States. MMWR. 2014, 63(SS02);1-21.
5. Davis NO, Kollins SH. Treatment for co-occurring attention deficit/hyperactivity disorder and autism spectrum disorder. Neurotherapeutics 2012; 9:518–530. doi:10.1007/s13311-012-0126-9.
6. Andersen PN, Hovik KT, Skogli EW, Egeland J, Øie M. Symptoms of ADHD in Children with High-Functioning Autism Are Related to Impaired Verbal Working Memory and Verbal Delayed Recall. PLoS One 2013; 8(5): e64842. doi: 10.1371/journal.pone.0064842
7. Yerys, BE, Wallace GL, Sokoloff1 JL, Shook DA, James JD, Kenworthy L. Attention deficit/hyperactivity disorder symptoms moderate cognition and behavior in children with autism spectrum disorders. Autism Res 2009; 2(6): 322–333. doi: 10.1002/aur.103.
8. Lee DO, Opal Y. Attention-Deficit Hyperactivity Disorder Symptoms in a Clinic Sample of Children and Adolescents with Pervasive Developmental Disorders. J Child Adolesc Psychopharmacol 2006; 16(6): 737–746. doi:10.1089/cap.2006.16.737.
9. Robison LM, Sclar DA, Skaer TL, Galin R. National Trends in the Prevalence of Attention-Deficit/Hyperactivity Disorder and the Prescribing of Methylphenidate among School-Age Children: 1990- 1 9 9 5 . C l i n P e d i a t r 1 9 9 9 ; 3 8 ( 4 ) : 2 0 9 – 2 1 7 . d o i : 10.1177/000992289903800402
10. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007; 164(6):942–48. doi: 10.1176/appi.ajp.164.6.942
11 . Wi l l c u t t E G . T h e p r e v a l e n c e o f D S M – I V a t t e n t i o n – d e f i c i t / h y p e r a c t i v i t y d i s o r d e r : a m e t a – a n a l y t i c r e v i e w. Neurotherapeutics 2012; 9:490–99. doi: 10.1007/s13311-012-0135-8
12. Gerralda ME, Rask CU. Somatoform and related disorders. In: Thapar A, Pine D (Eds) Rutter’s Child and Adolescent Psychiatry, 6th
edn. John Wiley & Sons, 2005, 1035-1054
13. Srinath S, Bharat S, Girimaji S, Seshadri S. Characteristics of a child inpatient population with hysteria in India. J Am Acad Child Adolesc Psychiatry 1993; 32(4):822-5. http://dx.doi.org/10.1097/00004583- 199307000-00017
14. Shaw P, Sporn A, Gogtay N, et al. Childhood-onset schizophrenia: a double-blind, randomized clozapine-olanzapine comparison. Arch Gen Psychiatry 2006; 63(7):721–730. doi:10.1001/archpsyc.63.7.721.
15. Maloney AE, Yakutis LJ, Frazier JA. Empirical evidence for psychopharmacologic treatment in early-onset psychosis and schizophrenia. Child Adolesc Psychiatr Clin N Am 2012; 21(4):885–909. doi: 10.1016/j.chc.2012.07.011.
16. Costello JE, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry 2006; 47(12):1263-
71. doi 10.1111/j.1469-7610.2006.01682.x
17. Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci 2009;
11(1):7–20
***



