METABOLIC SYNDROME AND ITS RELATIONSHIP WITH NEGATIVE SYMPTOMS IN FEMALE PATIENTS WITH SCHIZOPHRENIA
Abstract
Introduction: High prevalence of metabolic syndrome has been reported in patients with schizophrenia. Factors that contribute to the development of physical and biochemical abnormalities due to this syndrome are: sedentary lifestyle, antipsychotic medication, mental disorder related issues, including negative symptomatology and genetic factors. A significant association between negative symptoms, obesity and metabolic syndrome has been reported in recent studies. Objectives: The objectives of this study were to estimate the frecquency of metabolic syndrome and to examine the association between metabolic syndrome and negative symptoms in female patients with schizophrenia. Methods: Forty for female patients diagnosed with schizophrenia were recruited from psychiatric out-patient clinic. Patients underwent one assessment for metabolic syndrome parameters which included anthropometrical measurements, blood pressure, lipid profile, fasting plasma glucose level. The presence of the metabolic syndrome was determined using the International Diabetes Federation criteria. The Positive and Negative Syndrome Scale was used for characterising symptoms. Results: Mean duration of illness was 13.93 years and mean duration of education was 13.15 years. Metabolic syndrome was found in 52.27% of the patients (36% with hypertriglyceridemia, 86% with high waist circumference, 59% with low HDL cholesterol, 20.45% with high fasting glucose and 11% with hypertension. The frecquency of metabolic syndrome in group patients with predominant negative symptoms was significantly higher (p= 0.0026) compared to the group without predominant negative symptoms. Conclusions: Metabolic syndrome is common in female patients with schizophrenia. Systematically assessment of the various components of metabolic syndrome and adequate treatment should help to reduce the cardiovascular risk and mortality in patients with schizophrenia.
INTRODUCTION
Schizophrenia is a severe mental disorder characterized by positive symptoms (e.g. delusions, hallucinations), negative symptoms (e.g. flattened affect, lack of motivation, social withdrawal) and cognitive impairment, making it one of the first ten causes of chronic disability worldwide with burden in multiple aspects of social, family and professional life (1, 2).
Life expectancy for schizophrenia patients is 15-
20 years shorter, and the mortality rate is 2.5-3 times higher compared to the general population correlated with somatic pathology (3, 4). Cardiovascular pathology is the main cause of mortality among patients with schizophrenia (5, 6). According to the third report of the NCEP, metabolic syndrome is an important risk factor for cardiovascular disorders (7). The metabolic syndrome increases the relative cardio-vascular risk by 1.2-2 times (8).The metabolic syndrome is a conception that include hyperglycemia, increased blood pressure, elevated triglyceride levels, low high-density lipoprotein cholesterol levels and central obesity (9).
The exact prevalence of metabolic syndrome in patients with schizophrenia is not known, ranging between 11-69 % in treated patients and between 4-26 % in untreated patients; one in three patients fulfill the metabolic syndrome criteria and one in two patients is overweight (10).
The prevalence of individual factors that define metabolic syndrome was described byMitchell et al. in a metaanalysis of 126 studies including 25 692 patients with mean disease duration of 10.4 year: 9.4 % overweight patients,1 9.5 % patients with hyperglycemia,
39.3% with hypertriglyceridemia and 42.6 % with low levels of HDL – Cholesterol, 38.7 % with hypertension , and 10.9% with diabetes (7) .
Risk factors for metabolic syndrome and cardiovascular disorders in people with schizophrenia are complex; they can be divided into three categories: behavioral factors including lack of sufficient physical activity, smoking, substance abuse and unhealthy eating patterns; disease related factors with cardio-metabolic side effects of antipsychotic treatment and low socioeconomic status (11). Also, genetic factors contribute to the high prevalence of metabolic syndrome in these patients (12).
The negative symptoms, including a reduction of emotional responsiveness, motivation, socialization, speech and movement are included in behavioral factors which contribute to a higher risk of metabolic syndrome in patients with schizophrenia. A significant association association between negative symptoms, obesity and metabolic syndrome has been reported in recent studies (10, 11, 12).
The objectives of this study were to estimate the frequency of metabolic syndrome and to examine the association between metabolic syndrome and psychiatric symptoms in female patients with schizophrenia. MATERIALAND METHODS
44 adult female patients (age 18-55) with DSM- IV-TR and ICD-10 diagnosis of schizophrenia followed up in the outpatient service of the University Clinic of Psychiatry, Cluj-Napoca, Romania were included into the study. All patients had a minimum of 8 years of education. Patients were included if (a) acute symptoms were remitted, with no relapse in the last 6 months, (b) patients were stable on antipsychotic medication, using the same dosage for at least 4 weeks before inclusion. Patients were excluded if (a) they had a DSM-IV-TR diagnosis of alcohol dependence or other substance dependence, dementia, mental retardation, history of head trauma, or any current severe medical condition (cardiovascular, neuromuscular or endocrine condition)‚ (b) severe cardiovascular disorders diagnosed prior to the diagnose of schizophrenia.
The study was approved by the University of Medicine and Pharmacy Iuliu Hatieganu Ethics Committee and all patients signed an informed consent before being admitted in the study.
Information on age, education, economic status, tabacco smoking status, onset and course of illness, antipsychotic treatment were collected through the clinical interview. The types of antipsychotics were categorized into „clozapine /olanzapine” group and „other antipsychotics” group considering that clozapine and olanzapine may have a higher potential in generating metabolic abnormalities (20). Patients were also assessed for psychopathology using Positive and Negative S y n d r o m e S c a l e a n d r e c e i v e d a n t h r o p o m e t r i c measurements and a fasting metabolic laboratory screening. The definition for predominant negative symptoms used in this study suggests a baseline score ≥4 on at least 3 or ≥ 5 on at least 2 of the 7 negative subscale items and a PANSS positive score of <19. Sitting blood pressure, systolic (SBP) and diastolic (DBP) were recorded. Waist circumference was measured midway between the lowest rib and the iliac crest. Overnight fasting blood was collected for metabolic profile analysis: fasting level of serum triglyceride (TG), fasting plasma glucose level and serum high-density lipoprotein cholesterol (HDL-Col) level were measured. The diagnosis of metabolic syndrome was defined according to the modified criteria of the International Diabetes Federation (IDF) , which requires the presence of three or more of the following five criteria: high waist circumference (>94 cm for men and >80 for women), hypertrygliceridemia (>150 mg/dl or on lipid lowering medication), low HDL cholesterol level(<40 mg/dl in men and <50 mg/dl in women), high blood
pressure (≥ 130/85 mm Hg or on antihypertensive medication) and high fasting glucose concentration (≥100 mg/dl or on glucose-lowering medication) (9).
The association between clinical and demographic characteristics and metabolic syndrome was performed using chi square and Student’s t test. ANOVA test was used to describe the relationship between each component of metabolic syndrome characteristics and clinical and demographic characteristics.
RESULTS
The mean age of the patients was 40.45 years and the mean age of education 13.15 years. The mean duration of illness was 13.93 years. 17 patients (38.63%) were current tobacco smokers. The mean PANSS total score was 63.81, which indicates that symptomatology in the study group was mild. 47.72 % of patients had predominant negative symptoms.
Metabolic syndrome was found in 52.27 % of patients (86% with high abdominal circumference, 59% with low HDL cholesterol, 20.45% with high fasting glucose and 11% with hypertension). Female patients with metabolic syndrome had significantly lower education level (p=0.0017) and a significantly higher duration of illness (p=0.0014) compared to patients without metabolic syndrome. Metabolic syndrome was also found to be associated with olanzapine or clozapine current treatment (p=0.0002). The PANSS negative score was significantly higher in patients with metabolic syndrome (p=0.0079).
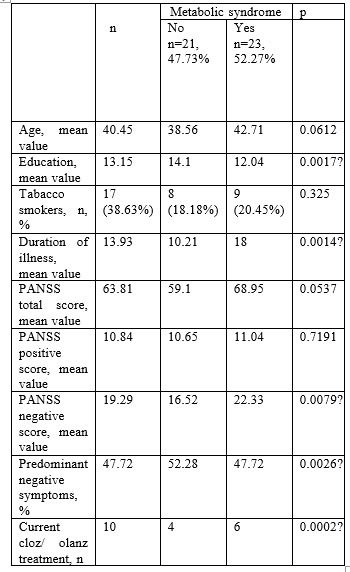
P<0.05- statistically significant
Table 1. Demographical and clinical characteristics of the
44 patients with schizophrenia and association with metabolic syndrome (MetS)
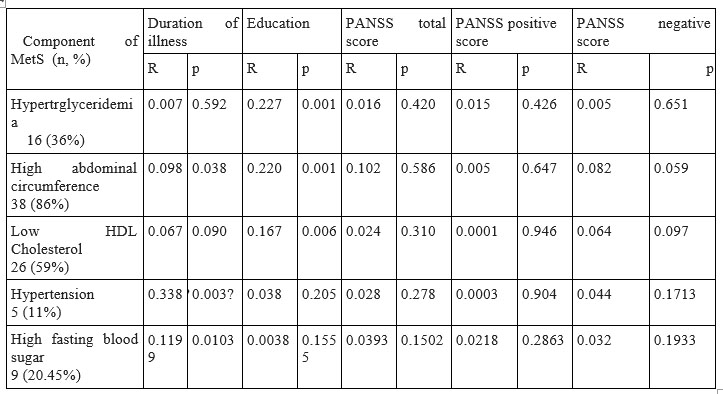
p<0.05 and R>0.25- positive correlation exists and it is statistically significant
Table 2 Correlations between components of metabolic syndrome and demographical and clinical characteristics
Investigating correlations between components of metabolic syndrome and clinical and demographical characteristics, it was found that hypertension has positive correlated significantly with duration of illness.
The frecquency of metabolic syndrome in group patients with predominant negative symptoms was significantly higher (p= 0.0026) compared to the group without predominant negative symptoms.
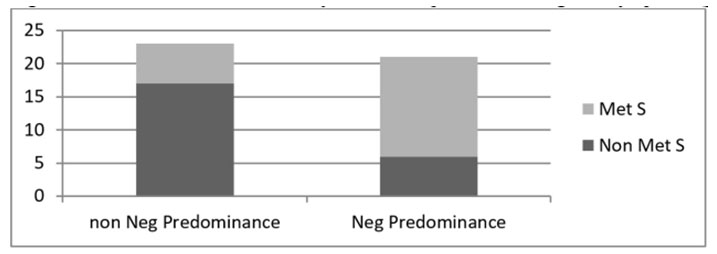
Fig 1 Association between metabolic syndrome and predominant negative symptoms (p=0.0026)
Predominant negative symptoms were found to be associated with higher abdominal circumference (p=0.025). No other component of metabolic syndrome was associated with predominant negative symptoms.
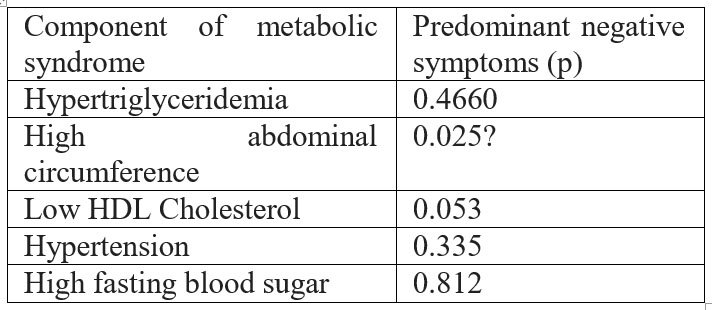
P<0.05- statistically significant
Table 3 Association between components of metabolic syndrome and predominant negative symptoms
DISCUSSIONS
This study assessed the frequency of metabolic syndrome in a Rumanian group of women patients diagnosed with schizophrenia, with mild symptomatology. In this sample, a high frequency of
52.27% of metabolic syndrome was observed, despite the fact that this sample was young (mean age 40.48 years). The prevalence of metabolic syndrome in female patients with schizophrenia is not known, ranging between 11-
69% in treated patients. Compared with literature data, the metabolic syndrome rate in this sample was higher, Clamors study reported a prevalence of 27.2%, and CATIE study reported a prevalence of 36% (19, 20). The higher rate of metabolic syndrome found in this study may be due to a worse dietary lifestyle and medical care factors, but may also reflect differences in sample characteristics and limited sample size.
In this sample, a frequency of 86% of high abdominal circumference, a frequency of 59% of low H D L C h o l e s t e r o l , a f r e q u e n c y o f 3 6 % o f hypertriglyceridemia, a frequency of 11% of hypertension and a frequency of 20.45% of high fasting glucose were observed. The results were also higher than those reported by Michell et al. in a recent meta-analysis performed on 25 692 patients: 39.3% hypertriglyceridemia, 42.6% with low levels of HDL-cholesterol and hyperglycemia 10.9% (7). Only hypertension was found in a small number of patients in our sample compared to the percentage of 38.7 reported by Michell and al.
A high percentage of patients following treatment with Olanzapine or Clozapine (60%) met the criteria for metabolic syndrome. Metabolic disturbances caused by olanzapine and clozapine are documented by meta-analyses. They are regarded as the most important antipsychotics that cause weight gain, hyperglycemia and dyslipidemia (21).
In this study, there were no significant differences between the metabolic syndrome group and the group without metabolic syndrome group regarding smoking habit and economic level. The rate of smokers found in this sample (37%) was 2.5 fold higher than the rate of
14.4% of female smokers in Romanian population (21). The results are consistent with the literature data which shows that smoking prevalence is almost three times higher among patients with schizophrenia compared with the general population and the number of cigarettes smoked is higher among patients with schizophrenia compared with the general population (22). In a Finnish study conducted in subjects with psychotic pathology, the habit of smoking was described as the most important predictors of mortality to 8 years (23).
Negative symptoms like anhedonia, apathy, associability, decreased interest in their own health, lack of motivation are factors related to lifestyle (diet, physical activity) involved in the etiology of metabolic syndrome. In this study, almost half of patients had predominant negative symptoms (47.72%). The frequency of metabolic syndrome is significantly higher in patients with predominant negative symptoms compared to the group without predominant negative symptoms. Also, abdominal circumference was significantly higher in patients with predominant negative symptoms. Literature data regarding the relationship between the type of symptomatology and metabolic syndrome disturbances are limited and inconclusive. Saddichha et al. (24) and Kirkpatrick et al. (25) showed that negative symptoms correlated with obesity and metabolic syndrome. In a recent study of 1120 patients, 52.2% were found with negative symptoms; the prevalence of metabolic syndrome was significantly higher in the group of patients with negative symptoms (43.9%) compared to the group without negative symptoms (34.9% 0) (26). Metabolic syndrome was significantly correlated with negative symptoms, age and somatic comorbidities. In a study of
372 patients with schizophrenia treated with antipsychotic a longer period of 2 years, Chen et al. showed that negative symptoms were negatively correlated with body mass index and serum triglyceride level and positively with HDL-Col level, authors suggesting that patients with negative symptoms may have a different lipid profile compared to those with no obvious negative symptoms (27). Other studies did not find significant differences in negative symptomatology between patients with and without metabolic syndrome (19).
When the relationship between negative symptoms and metabolic disturbances was investigated, various definitions were choose for negative symptoms. This is one of the reason for the inconclusive conclusions in literature. Future studies and meta-analysis are needed in this field of study.
This study has several limitations. Due to the cross sectional nature of the study, we were unable to investigate the causal nature of the differences observed between the two groups (with and without metabolic syndrome) and also of the associations found between negative symptomatology and metabolic syndrome components. The small sample size is another limitation of this study.
CONCLUSIONS
This study demonstrates that metabolic syndrome and its components (dyslipidemia, obesity, hyperglycemia, hypertension) had a high frequency among young female patients with mild and stable symptoms of schizophrenia compliant to atypical antipsychotics treatment.
Almost half of the study group had predominant negative symptoms. Metabolic syndrome was diagnosed significantly more often in patients with predominant negative symptoms.
These findings highlight the need for systematically anthropometric and biochemical evaluation in order to early detect the metabolic disturbances in patients with schizophrenia. The prevention and treatment of metabolic syndrome should help to reduce mortality and to improve overall prognosis in this population.
ACKNOWLEDGEMENTS
All the authors had an equal contribution and have similar rights. All the authors approved the final version of this article.
DISCLOSURES: The authors report no conflict of interest for this article.
LIST OF ABREVIATIONS:
PANSS- positive and negative syndrome scale
MetS- Metabolic syndrome
NCEP- National Cholesterol Education Program
HDL- High density lipoprotein
REFERENCES
1. Rossler W, Salize HJ, Van OJ, Riecher-Rossler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol 2005; 15:399–409.
2. Rutz W. The European WHO mental health programme and the World Health Report 2001: input and implications. Br J Psychiatry 2003;183:73–4.
3. Mc Grath, J., Saha, S., Chant, D., Welham, J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 2008; 30:67-76.
4. Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123-31.
5. Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150(6):1115-21.
6. Shoesmith WD, Al Mamun M, Abdulah AF, Naing DKS, Turin PT. Cardiovascular diseases among patients with schizophrenia. Asian Journal of Psychiatry 2015; 19:28-36.6.
7. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of HighBlood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106(25):3143-421.
8 . Fleischhacker W, Cetkovich-Bakmas M, De Hert M. Comorbid somatic illness in patients with severe mental disorders: clinical, policy and research challenges. J Clin Psychiatry 2008; 69:514-519.
9. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome- a new word-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469-480.
10. Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders-a systematic review and meta- analysis. Schizophr Bull. 2013;39(2):306-18.
11. Vancampfort D, Wampers M, Mitchell AJ, Correll CU, De Herdt A, Probst M, De Hert M. A meta-analysis of cardio-metabolic abnormalities in drug naive, first-episode and multi-episode patients with s c h i z o p h r e n i a v e r s u s g e n e r a l p o p u l a t i o n c o n t r o l s . Wo r l d Psychiatry.12(3):240-50.
12. Malan-Müller S, Kilian S, van den Heuvel LL, Bardien S, Asmal L, Warnich L, Emsley RA et al. A systematic review of genetic variants associated with metabolic syndrome in patients with schizophrenia. Schizophr Res. 2016;170(1):1-17.
13.Rummel-Kluge C, Komossa K, Schwarz S,Hunger H, Schmid F,21. Ministerul Sanatatii. Retrieved Aprilie 26, 2016, from Lobos CA, et al. Head-to-head comparisons of metabolic side effect s of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta- analysis. SchizophrRes 2010; 123:225–33.
14. Saddichha S, Ameen S, Akhtar S. Predictors of antipsychotic induced weight gain in first episod psychosis:conclusions from a randomised double blind controlled prospective study of olanzapine, risperidone and haloperidole. Journal of Clinical Psychopharmacology 2008a;28:27-31.
15. Kirkpatrick B, Fernandez-Egea E, Garcia-Rizo C, Bernando M. Differences in glucose tolerance between deficit and nondeficit schizophrenia. Scizophr Res 2009;107:122-127.
16. Meyer JM, Nasrallah HA, McEvoy JP, Goff DC, Davis SM, Chakos M et al. The Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial: clinical comparison of subgroups with and without the metabolic syndrome. Schizophr Res 2005; 80: 9–18.
17. Stauffer VL, Song G, Kinon BJ, Ascher-Syanum H, Chen L, Feldman PD, Conley RR. Responses to antipsychotic therapy among patients with schizophrenia orschizoaffective disorder and either predominant and proeminent negative symptoms. Schizophr Res 2012;134(2-3):195-201.
18. Nasrallah HA. Metabolic findings from the CATIE trial and their relation to tolerability. CNS Spectr 2006;11(7 Suppl7):32–9.
19. Bobes J, Arango C, Randa P, Carmena R, Garcia-Garcia M, Rejas J. Cardiovascular and metabolic risk in outpatients with schizophrenia treated with antipsychotics: results of the CLAMORS Study. Schizophr Res. 2007;90(1-3):162-73.
20. Rummel-Kluge C, Komossa K, Schwarz S,Hunger H, Schmid F, Lobos CA, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta- analysis. SchizophrRes 2010; 123:225–33.
21. Ministerul Sanatatii. Retrieved Aprilie 26, 2016, from http://www.ms.ro/?pag=62
22. DeLeon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. SchizophrRes 2005;76:135–57.
23. Suvisaari J, Partti K, Perälä J, Viertiö S, Saarni SE, LönnqvistJ ,etal. Mortality and its determinants in people withpsychotic disorder. PsychosomMed 2013;75(1):60–7.
24. Saddichha S, Ameen S, Akhtar S. Predictors of antipsychotic induced weight gain in first episod psychosis:conclusions from a randomised double blind controlled prospective study of olanzapine, risperidone and haloperidole. Journal of Clinical Psychopharmacology 2008a;28:27-31.
25. Kirkpatrick B, Fernandez-Egea E, Garcia-Rizo C, Bernando M. Differences in glucose tolerance between deficit and nondeficit schizophrenia. Scizophr. Research 2009;107:122-127.
26. Sicras-Mainar A, Maurino J, Ruiz-Beato L, Navarro-Artieda R.Prevalence of metabolic syndrome according to the presence of negative symptoms in patients with schizophrenia. Neuropsychiatr Dis Treat 2015;11:51-57.
27. Chen SF, Hu TM, Lan TH, Chiu HJ, Sheen LY, Loh EW. Severity op psychosis syndrome and change of metabolic abnormality in chronic schizophrenia patients: Severe negative syndrome may be related to a distinct lipid pathophysiology.European Psychiatry 2015;29:169-171.
***