THE IMPORTANCE OF THERAPEUTIC ALLIANCE FOR THERAPY PROGRAMS USED IN ONSET SCHIZOPHRENIA SPECTRUM DISORDER
Abstract
Background: Therapeutic alliance is considered an important therapeutic factor for both the success in the act of therapy, but also for the involvement of the patients. Objectives: our study intends to evaluate therapeutic alliance for patients undergoing a psychotherapeutic intervention from an existential analytical approach, during one year at least, after the first episode of schizophrenia. Material and Methods: We conducted a pilot study of p ro s p e c t i v e - l o n g i t u d i n a l d e s i g n , i n v e s t i g a t i n g effectiveness of existential analytical psychotherapy interventions in patients after a first episode of psychosis, by comparing two groups (experimental and control) of subjects. In this paper, we present the results from the experimental group, clinical evaluated with PANNS and CGI-S, and functional with GAFS. The therapeutic alliance was evaluated with the Revised Helping Alliance Questionnaire (HAq-II revised) –the patient version. Results: The analysis of median values in scores for HAq- II, at baseline were of 88,61, grew at 6 months at 92,09, and at 12 months at 95,06, for the patients maintained in the study (n=17). There were significant statistical differences between the two groups for these scores at baseline, as the Mann-Whitney test shows (p=0,005), maintaining at 6 months (p=0,006). Conclusions: From the beginning of the program, establishing a good therapeutic alliance with patients after a first episode schizophrenia, in psychotherapy interventions with an existential analytical approach is possible. This strong client - therapist relationship will lead to a persistence in therapy with good results on symptomatic and functional outcome.
T H E R A P E U T I C A L L I A N C E A N D P S Y C H O L O G I C A L
I N T E R V E N T I O N I N SCHIZOPHRENIA SPECTRUM DISORDERS
The first five years in schizophrenia evolution are considered the most important and throughout this perspective, early and sustained interventions are a major objective for these patients well-being. According to guides, these early interventions are a combination of psychopharmacological approach and psychosocial interventions. In fact though, involving patients with schizophrenia spectrum disorders and maintaining them in therapy is a real challenge, and this process has often a high rate of abandonment, followed shortly by relapse (1, 2).
Therapeutic alliance is consider an important therapeutic factor for both the involvement of patients, but also for the success of the therapeutic program itself, which is explained by a reduced severity in symptomatology, a better treatment compliance, low rates of drop-out and fewer hospitalizations (3, 4). The therapeutic relationship is dependent on a variety of factors of which some are of client’s interest, while others are of therapist interest.
Most studies evaluating therapeutic alliance were conducted in standardized therapeutic programs, which include cognitive-behavior therapy (CBT) and recovery- oriented cognitive therapy (CT-R) (5, 6, 7), and they investigated patients with a long history of disease. In these cases, therapeutic alliance could be influenced by previous negative experience with other treatments. These studies focus on factors patient-dependent and are targeting the predictive value of positive symptoms, insight and social abilities. The results are partially contradictory, as regarding the severity of positive symptomatology, which correlates negative, in some studies, with how the therapeutic alliance is perceived by the patient, while in others they do not (5, 8, 9). The same contradictory results appear when the patient, and also the therapist opinion on the quality of therapeutic relationship were investigated. Some studies reported significant associations between their opinion and how good the relationship was (8, 9, 10), while others did not find an association (11), and some studies reported a higher significant rates for the relationship perceived by the patient (8, 9). Regarding insight, this factor correlates, in most studies, with a good therapeutic relationship, as perceived by the patient (5, 8, 11). Cognitive factors don’t seem to influence in any way the client-therapist relationship, but there are some studies that report a correlation with its alliance importance for the therapist (10).
There are few studies to investigate therapeutic alliance at the onset of schizophrenia. One of these studies evaluated therapeutic alliance in these patients, while undergoing a group therapy intervention (1). High variations in therapy alliance levels appear in patients with worsening negative symptomatology, after therapeutic intervention. Of all the variables assessed that could influence this outcome, only patient attachment, measured at baseline is predictable for how general scores of both clients, and therapist will evolve, and between these two variables there is also correspondence. Due to group intervention specifications, the results are hard to generalize to other forms of psychotherapeutic approaches. In another transversal study (12), patients with high education level have higher score on therapeutic alliance scales. The presence of positive symptomatology was correlated negatively with the level of alliance from the patient point of view, while insight correlated with therapist scores for alliance. Neurocognitive factors have no influence in therapy alliance also in this study. Another study, whose aim was to describe a patients profile difficult to engage in psychiatric therapy and with a low treatment adherence, at the onset of schizophrenia (13), found correlations between childhood traumatic history and a low ability to establish relations, meaning also therapeutic relationship. In other words, subjects who were directly involved or witnessed family violence develop an unsecure form of attachment, with difficulties in seeking help and maintaining relationships, which predicts a lower level of therapeutic alliance, translated as a weaker engagement in the therapeutic process.
Research done in the field of psychotherapy (14, 15) shows that the results obtained are depending on the quality of the psychotherapeutic relationship, which means that a week alliance is correlated with the end of therapeutic relation, made by patient. Last year’s main focus research lead to a preoccupation in identifying the factors that influences most the client-therapist relationship, especially the maintaining, rupture and repairing of the relationship. The factors that prevailed were shared opinion about the course of therapy, emotional bounds, including negative emotions or disagreement in establishing objectives (16). Any kind of communication throughout the course of therapy should be followed by feed-back, from the interlocutor perspective. In the particular case of clients with psychotic disorders, as a consequence of subjectivity and poor insight, this act requires a delicate approach, but also honesty on behalf of the therapist.
From the perspective of factors that are most relevant for therapeutic alliance and are therapist dependent, two studies that review literature data (17, 18) identify that a therapist perceived as warm, empathic and friendly is positive correlated with a better therapeutic alliance; while a superficial, critical and non-responsive therapist correlates negatively with the relationship. A more recent CBT for patients with psychosis study (19) tries to identify the specific characteristics of the therapist, predictive for good therapeutic alliance, and suggest that the most important factor is how authentic the therapist is perceived by the patient. This is in fact, no novelty in the field, since in the ’50, Carl Rogers considered that therapist-dependent factors like unconditioned positive attitude, empathy and authenticity, as being the nucleus for good therapeutic alliance.
OBJECTIVES
The aim of this present study is to evaluate therapeutic alliance for patients after a first episode of schizophrenia, undergoing a psychotherapeutic intervention existential analytical approach, during at least one year. The results presented belong to the therapeutic group, from a pilot prospective longitudinal study investigates the effectiveness of this type of psychotherapeutic approach, in onset schizophrenia, comparing two sets of subjects divided in two groups, an experimental and a control group, and its belong to the experimental group. For this reason we tried to answer the following questions:
-Does symptomatology in the onset of schizophrenia patients influence the development of therapeutic relationship?
-Are there any correlations between the length of untreated psychosis and therapeutic alliance?
-Does the quality of therapeutic relationship impact persistence in therapy or the drop out-rates?
Based on previous studies we assumed that the level of therapeutic alliance will correlate adversely with the severity of positive symptomatology and will not be influenced by the negative one or the length of untreated psychosis. Another hypothesis was the fact that a good therapeutic alliance from the beginning of the program will be associated with a high maintenance level in therapy and the reverse situation where a poor one will lead to abandonment.
METHODS
Study design: Subjects were recruited from hospitalized patients of “Prof. Dr. Al. Obregia” Psychiatric Hospital, in Bucharest, toward the ending of hospitalization or just after discharge. Patients were been diagnosed with first episode of psychosis/ acute psychotic disorder with schizophrenia symptoms/schizophrenia. There were two patients referred from ambulatory services, who were never been hospitalized. The recruitment was done between 2009 and 2012. The study was approved by the Ethical Committee for the hospital. For the experimental group, we establishing a year length for follow up study, with intention to maintain the therapy for 2 years, based on previous study observations (20), which states that a more stable symptomatology and a functional recovery appears only after a period of 1 year therapy and, in the second year, improvement is going on.
Procedure.
Analytical Existential intervention, which involve counseling and supportive therapy were performed by only one therapist. Patients from the experimental group participated in weekly sessions, with a 40-50 minutes length, on the course of 2 years. After the 4-th session, we applied HAql revised- patient version, this being considered as baseline time. We were mainly interested in the patient version of the test, since this is the one who expresses subjective perspective on the therapeutic relationship from the client perspective, and studies outlined its importance in the stability of the relationship, and possible rupture (16). The scale was applied also at 6, 12, 18 and 24 months. Clinical evaluations were performed using PANNS, CGI and functional assessment was done on a GAF scale, by an experienced clinical psychologist, blinded for the patient’s affiliation group. These tests were also performed at the patient’s adherence to the study, but also at 6, 12, 18 and 24 months.
Subjects. Inclusion criteria were: age between
16 and 35; fulfillment of all diagnostic criteria for schizophrenia spectrum disorder, after a first episode, according to DSM –IV; after applying clinical structured interview diagnose (SCID), in stable patients, who are under psychotic treatment. Exclusion criteria gathered the following: history of cerebral damage, traumatic or infectious cerebral injuries, neurological disease or mental retard (IQ<70) and the use of psychoactive substances.
Patients were at most diagnosed in the previous year of their study inclusion with psychotic spectrum disorder and were undergoing antipsychotic medications, which were maintained throughout all study period. All patients admitted in the study signed a consent form. Inclusion and exclusion criteria were established based on literature data (21, 22), which outlined the importance of sustained antipsychotic treatment, after a first schizophrenia episode and the facilitating role of psychological interventions in reaching and maintaining symptomatic remission and functionality, but also recovery for these patients.
Off all 118 subjects referred in the study, 39 of them didn’t accomplish the inclusion criteria and 33 refused signing the consent form. The 46 subjects who reached baseline were distributed alternatively, in the lots, experimental or control, leading to a 23 patients in each group, with the same sex distribution. In this paper, we present the results from the experimental group.
M e a s u r e m e n t t o o l s . WA S I ( We c h s l e r Abbreviated Scale of Intelligence) – is a shorter version, similar to WAIS –III (a revised version on ’97 WAIS), which allows clinicians to estimate verbal IQ scores, performance IQ and global IQ, in a shorter period of time. The scale was applied before entering the study; results lower than 70, being considered exclusion criteria.
For clinical assessment we used PANNS and CGI-S. PANSS (Positive and Negative Syndrome Scale) was developed by Kay et all. (23) for the measurement of psychopathology severity in adults with schizophrenia, schizophrenia disorders and other psychosis. The psychometric characteristics of PANNS are good, with a good internal consistency; of above 0.75, but with variability between each applier, based on his experience in applying the test. In our case, variability is low because the scale was applied by only one interviewer, throughout the whole study. CGI (Clinical Global Impression Scale) is used for more than 30 years in clinical studies, offering a rapid evaluation of various aspects regarding the disease, at a certain point. The information evaluated is: patient history, psychosocial circumstances, symptoms and behavior, as well as their impact on functionality (24). The scores obtained correlates with PANNS results (25, 26).
Functional evaluation was done using Global Assessment of Functioning Scale (GAFS). Although there are a series of problems related to the scale, as it’s concerning validity and reliability, due to the absence of comprehensive guides for GAF scoring, which leads to confusion (27), some studies sustain that the scale is valid and sensitive to change, especially if we use it at repeated, short periods of time (months) in the course of the disease (28). In this study we registered scores of functionality GAF-F. Despite recent DSM 5 changes, APA still recommends the usage of the scale for functional assessment (29).
Revised Helping Alliance Questionnaire – HAqII-r (patient version) is a revised version of one of the first and most utilized questionnaires for evaluating therapeutic alliance, which was done in 1996, by Lester Luborsky et all. (30). At its origins are Penn scales, created on the psychodynamic concept of Luborsky therapeutic alliance (1984), which measures two types of signs: type I, client’s experience with the therapeutically relationship, as a helping one ; type II, intervention experience of the client, as a process in which he works together with the therapist for reaching common objectives. This version (30) has been demonstrated to be better associated with the construct of therapeutic alliance and is less influenced by patient’s symptoms. The scale, in its last version captures, especially, aspects related to emotions and emotional bonds, based on trust, respect and understanding. The questionnaire comprises 19 items. The scale has answers on which both the client and therapist reports to, choosing the right version of response for them on a Likert scale, from 1 to 6, from strongly disapprove to completely agreed. In the present study we used only the patient version applied without a time limit. We calculated a final score on each version, and considered values lower than 86 to be week alliances. Some authors (31, 32) consider that this test scores are sensible to predicting therapy results, which correlates with the level of patient satisfaction with treatment, and less with symptoms improvements. The test is easy to administer, needing only a 10 minutes period of administration. The author’s reports a good internal consistency and reliability.
Statistical analysis was done using SPSS (Statistical Package for Social Sciences), version 20. Testing normal distribution of variables was done by Kolmogorov-Smirnov test. Due to drop-out rates which lead to a minimize group, beyond 12 months evaluation, especially in control group and also absence of sufficient data for this lot, statistical analysis was performed at baseline, 6 and 12 months.
Evolution of scores analyzed, on symptomology and functionality scales was done using multivariable statistical model – General Linear Model – GLM Repeated Measures – for comparing scores variation of the same subjects in time (at baseline, 6 and 12 months). In order to test our hypothesis, we calculated correlations between HAqII –patient version at baseline and patient characteristics from the experimental group, with rho’s Spearman correlation coefficient. Using Mann-Whitney non-parametric test we compared scores means on HAqII -scores at baseline and 6 months for those patients who remained in therapy for twelve months, with those patients who left the study after 6 months. We considered a p value of 0.05 as level of statistical significance.
RESULTS
The experimental group consisted of 23 patients,
17 were males (73,9%) and 6 females (26,1%). Mean age was 25,04 (±4,139) years , mean school level was 13,22 (±2,746) years and mean period of untreated psychosis 1 0 , 3 ( ± 1 0 , 4 4 2 ) m o n t h s . S o c i o – d e m o g r a p h i c characteristics and baseline variables in the experimental group are presented in Table 1. At 6 months we obtained results from 22 patients included in the study (95,6%) and at 12 months from only 17 (73,9%).
Results at 18 and 24 months were evaluated for only 7 patients, left in the study (30,4%). (DUP), and IQ (intelligence coefficient).
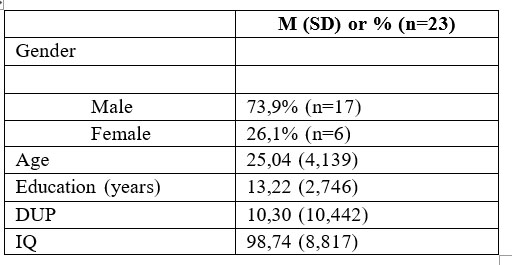
Table 1. Socio-demographic characteristics at baseline, duration of untreated psychosis (DUP), and IQ (intelligence coefficient)
S i g n i f i c a n t i m p r o v e m e n t s r e g a r d i n g symptomatology were registered for PANNS scores, both positive and negative, but also for CGI-S, at 6 months, (p<0,001). These scores continued to improve for the next period evaluated, in a similar way compared to the baseline. Variations in PANNS scores was low for positive symptomatology (p=0,002), between 6-12 months, compare to the first period baseline-6 months, and is associated with a similar CGI-S variation evolution (p=0,002). For the functionality evaluated with GAF, improvements also, with statistic signification observed between baseline-6 months, and 6 months-12 months (p<0,001). The results for PANSS positive and negative, CGI-S analysis, and GAF’s functionality, analyzed with General Linear Model Repeated Measures, are presented in table 2.
General Linear Model Repeated Measures – Pairwise comparisons, in three moments: baseline, 6 months, and 12 months.
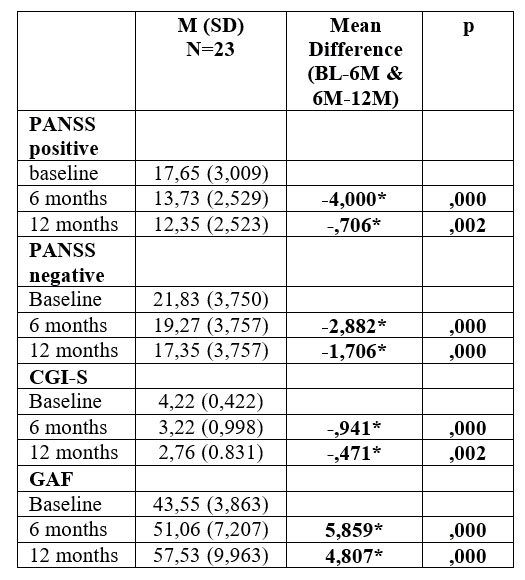
*p<0.05
Table 2. Symptomatology (PANSS and CGI-S), and global functioning (GAF) analysis with General Linear Model Repeated Measures – Pairwise Comparisons, between 6 months to baseline, and 12 months to 6 months.
Therapeutic alliance mean scores at baseline on HAqII – patient version were 88,61 (±5,719), they grow at 6 months to 92,09 (±5,951) and then again, at 12 months to 95,06 (±9,634), for those patients who remained in the study (n=17). In the first 6 months, one patient is lost due to relapse, and between 6 months-1 year, we lose 5 more patients. When we look at mean scores in evolution, for patients who persist in therapy for a 1 year minimum (subgroup N1), and compare those results with the ones from patients who go out of the study after only 6 months (subgroup N2), we noticed that there is an important difference in scores at baseline, which has an influence on each of these subgroups. Mean scores on HAqII in each subgroup are presented in table 3.
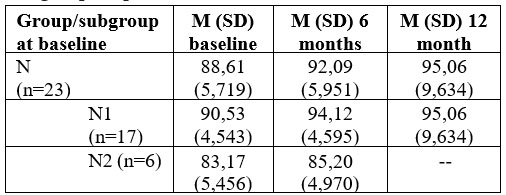
Table 3. HAqII-p.v scores results in each subgroup
For the subgroup of patients N2, who leave the study at 6 months (n=6), initial mean score on therapeutic alliance scale is lower, and does not improve after 6 months, while for patients who remained in the study for at least 1 year, noted N1 (n=17), baseline scores are higher and tend to improve after 12 months. Score differences in each subgroup are statistically significant at baseline (p=0,005), and it maintains at 6 months too (p=0,006). Comparing the groups was done using Mann-Whitney test; results are shown in table 4.
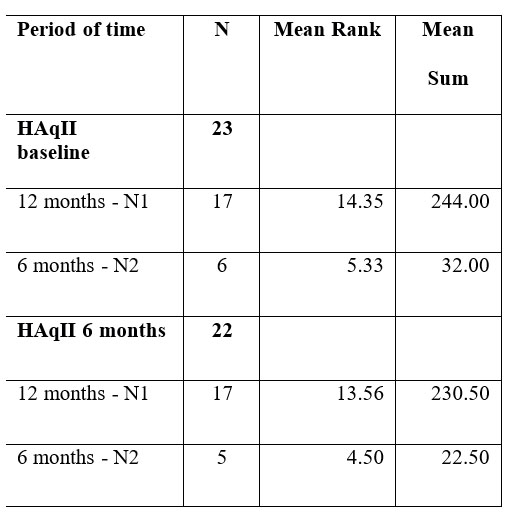
Test statistics (based on study period of time)
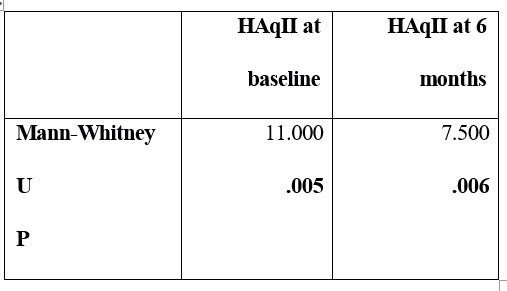
Table 4. Mann- Whitney test results comparing baseline and 6 months mean scores on HAqII for patients who remained in study for 12 months (N1), and for 6 months, only (N2)
The study revealed no statically significant differences in scoring alliance, based on gender influence. Also we found no correlations, at baseline, between HAqII-scores for alliance and other demographic variables, an neither between alliance scores and symptomatology scores at baseline, except positive PANNS which correlates negatively with values of scoring on HAqII, (p=0,018). Correlations were made using Spearman’s rho coefficient for non-parametric distributions as is shown in Table 5.
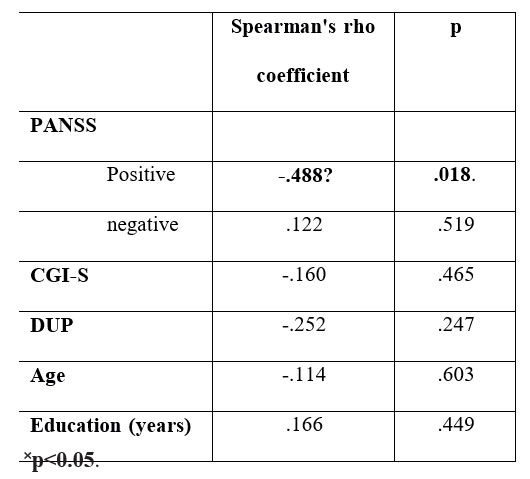
Table 5. Spearman’s rho coefficient at baseline (n=23) between HAqII-vp and patient symptomatology, DPN, demographic characteristics
DISCUSSIONS AND CONCLUSIONS
In our analyzed group, patients characteristics at baseline, including duration of untreated psychosis were not correlated with therapeutic alliance, with the exception of PANNS-positive score, which correlated negatively, meaning that high scores on PANNS-P, translated as positive symptoms predominance, are correlated with a low level of therapeutic alliance. From a clinical point of view this makes sense since a delusional patient, with a high degree of suspicion, perceives in a particular way the client-therapist relationship, as other studies have shown (10, 12). These are answers to the first and second questions, as objectives at present study.
Looking at our results we may say that there is an evident influence between the quality of therapeutic relationship from patient’s perspective and the course of therapy, in other words patients who obtained higher scores on HAqII-patient version, meaning a strong therapeutic alliance, persisted in therapy, with good results on symptomatic and functional outcome. An interesting observation is the fact that, in the case of patients with low scores from the beginning, in other words with a low alliance therapy scores (<86, according to questionnaire authors), these scores do not improve in time and patients will abandon therapy. This finding is concordant with Goldsmith et all. study results from 2015 (33), which demonstrates that there is a potential cause effect of therapeutic alliance in psychotherapy results for psychosis. More than that, the authors consider that establishing a good therapeutic alliance is essential for the patient, if he wants to profit from therapy results, and also that, maintaining in therapy a patient with week alliance is unfavorable for his recovery.
This research results suggest that establishing a good therapeutic alliance in analytical existential oriented therapy is possible, since the beginning of the program in patients at the onset of schizophrenia spectrum disorder, and this will lead to maintaining in therapy and obtaining desirable results;
the key ingredients for this to happened are not found in the disease itself or in the way an ill person manages to strive through it, indirectly objectified by functionality, the key to success is in the human’s nature itself, in the way he perceives the therapist as a vehicle of necessary guidance and in the way these meetings are organized, which depends more on the therapist, since relation difficulties tend to appear more often in people suffering from schizophrenia.
Alfried Längle (34) states that in existential analysis oriented therapy there is a particularity in the therapeutic meeting. The patient presents himself to the therapist with a help request to which the therapist responds by his professional competence. The core of the meeting is the patient and his problems, which he addresses to the therapist, and this assumes a sort of “being at this place one for the other”, in a most authentic kind, and in a partnership. The patient feel on behalf of the therapist, an “Yes” addressed to his dignity, his acceptance, said to his life. This “yes” become a common goal and thru this goal, they will build a strong bridge for therapeutic alliance. Metaphorically speaking, a relationship is stronger as partners are united thru the common goals and to this goal initiated first by the patient, the therapist responds by guidance thru therapeutic meeting.
This research has a series of limitations due, first of all, to the reduced number of patients, which caused a lower impact significance of the statistics analysis and did not allowed evaluation of possible effect size and interactions, and so the possibility of other co- occurring factors, not fully specified by this research, was not excluded. Another limitations was caused by the chosen method of gathering data at baseline (after the 4 meting), which can lead to insufficient data regarding the way a therapeutic alliance is established at the beginning of the intervention program. Using the previous idea as a starting point, we suggest that, perhaps, a more reliable method for describing how a client-therapist relationship is build, could be better assessed thru data evolution after every meeting, in the first 10 meetings.
Another study limitation was caused by the fact that information about therapy alliance were gathered only from patients, not therapists. This limitation was imposed thru the study design, in which we involved only one therapist, in this manner emphasizing the patient perspective. By involving multiple therapists, the study would have gain heterogeneity by adding supplemental data to the equation from describing favorable characteristics of establishing a good client – therapist partnership in this patients. This approach will be observed in future studies.
REFERENCES
1.Lecomte T, Laferriere-Simard M-C, Leclerc C. What does the alliance predict in group interventions for early psychosis? Journal of Contemporary Psychotherapy. 2012;42: 55-61
2.Bourdeau G, Theroux L, Lecomte T. Predictors of therapeutic alliance in early psychosis. Early intervention in psychiatry 2009;3: 300-3
3.McCabe R, Bullenkamp J, Hansson L, Lauber C et al. The therapeutic relationship and adherence to antipsychotic medication in schizophrenia. PloS One 2012;7(4): e36080.
4.Priebe S, Richardson M, Cooney M, Adedeji O, McCabe R. Does the therapeutic relationship predict outcomes of psychiatric treatment in patients with psychosis? A systematic review. Psychotherapy and psychosomatics 2011;80: 70-7.
5.Lysaker PH, Davis LW, Buck KD, Outcalt S, Ringer JM. Negative ymptoms and poor insight as predictors of the similarity between client and therapist ratings of therapeutic alliance in cognitive behavior therapy for patients with schizophrenia. J Nerv Ment Dis 2011;199: 191-5.
6.Svensson B, Hansson L. Therapeutic alliance in cognitive therapy for schizophrenic and other long-term mentally ill patients: development and relationship to outcome in an in-patient treatment programme. Acta psychiatrica Scandinavica 1999;99: 281-7.
7.Huddy V, Reeder C, Kontis D, Wykes T, Stahl D. The effect of working alliance on adherence and outcome in cognitive remediation therapy. J Nerv Ment Dis 2012;200: 614-9.
8.Barrowclough C, Meier P, Beardmore R, Emsley R. Predicting therapeutic alliance in clients with psychosis and substance misuse. J Nerv Ment Dis 2010;198: 373-7.
9.Catty J, White S, Koletsi M et al. Therapeutic relationships in vocational rehabilitation: predicting good relationships for people with psychosis. Psychiatry research 2011;187: 68-73.
10.Davis LW, Lysaker PH. Neurocognitive correlates of therapeutic alliance in schizophrenia. J Nerv Ment Dis 2004;192: 508-510.
11.Wittorf A, Jakobi U, Bechdolf A et al. The influence of baseline symptoms and insight on the therapeutic alliance early in the treatment of schizophrenia. European psychiatry : the journal of the Association of European Psychiatrists 2009;24: 259-67.
12.Johansen R, Iversen VC, Melle I, Hestad KA. Therapeutic alliance in early schizophrenia spectrum disorders: a cross-sectional study. Annals of Gen Psychiatry 2013;12: 14.
13.Lecomte T, Spidel A, Leclerc C, MacEwan GW, Greaves C, Bentall RP. Predictors and profiles of treatment non-adherence in services problems in early psychosis. Schizophrenia Research 2008; 102: 295- 302.
14.Horvath AO, Bedi, RP. The alliance. In: Norcross J.C. (Ed.). Psychotherapy relationships that work. New York, NY: Oxford University Press, 2002.
15.Samstag, LW, Mura JC, Safran JD. Defining and identifying alliance ruptures. In: Charman D. (Ed.). Core concepts in brief dynamic psychotherapy. Hillsdale, NJ: Erlbaum, 2004, 187–214.
16.Safran JD, Muran JC, Eubanks-Carter C. Repairing alliance rupture. Psychotherapy 2011;48: 80-87.
17.Ackerman SJ, Hilsenroth MJ. A review of therapist caracteristics and techniques negatively impacting the therapeutical alliance. Psychotherapy: Theory, Research, Practice Training 2001; 38: 171-185.
18.Ackerman SJ, Hilsenroth MJ. A review of therapist caracteristics and techniques positively impacting the therapeutical alliance. Clinical Psychology Review 2003;23: 1-33.
19.Jung E, Wiesjahn M, Rief W, Lincoln TM. Perceived therapist genuineness predicts therapeutic alliance in cognitive behavioural therapy for psychosis. British J. C. Psychology 2015;54: 34-48.
20.Rosenbaum B, Valbak K, Harder S et al. Treatment of patients with first-episode psychosis: two-year outcome data from the Danish National Schizophrenia Project. British J Psychiatry 2005;186: 394-399.
21.Penn DL, Uzenoff SR, Mueser KT et al. A Pilot Investigation of the Graduated Recovery Intervention Program (GRIP) for First Episode Psychosis. Schizophr. Res 2011;125(2-3): 247-256.
22.Guo X, Zhai J, Liu Z et al. Antipsychotic Medication Alone versus Combined with Psychosocial Intervention on Outcomes of Early Stage Schizophrenia: A Randomised, One-year Study. Arch Gen Psychiatry 2010;67(9): 895-904.
23.Kay SR, Fiszbein S, Opler LA. The Positive and Negative Sundrome
Scale (PANSS) for Schizophrenia. Schizophr Bull 1987;13: 261-276.
24.Busner J, Targum S. The Clinical Global Impression Scale: Applying a Research Tool in Clinical Practice. Psychiatry 2007;4(7): 29-37.
25.Rabinowitz J, Levine S, Martinez G. Concordance between measures of functioning, symptoms, and change: examining the GAF, CGI-S, CGI-I, and PANSS. J Clin Psychopharmacol 2010; 30(4): 478-480.
26.Leucht S. Measurements of Response, Remission, and Recovery in Schizophrenia and Examples for Their Clinical Application. J Clin Psychiatry 2014;75
(suppl 1): 8-14.
27.Aas M. Guidelines for rating Global Assessment of Functioning (GAF). Annals Of Gen Psychiatry 2011;10: 2-11.
28.Spitzer RL, Fleiss JL, Endicott J. Global Assessment Scale (GAS), Global Assessment of Functioning (GAF) Scale, Social and Occupational Functioning Assessment Scale (SOFAS). In: Rush AJ,
First MB, Blacker DB (eds). Handbook of Psychiatric Measures (2nd ed). Washington DC: American Psychiatric Publishing, Inc, 2008, 86–90.
29.Gold LH. DSM-5 and Assessment of Functioning: The World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0). J Am Acad Psychiatry Law 2014;42 (2): 173-181.
30.Luborsky L, Barber JP, Siqueland L et al. The Revised Helping Alliance Questionnaire (HAq-II) Psychometric Properties. J Psychother Pract. Res 1996;5(3): 260-271.
31.Le Bloc Y, Roten Y, Drapeau M, Despland JN. New but improved? Comparison between first and revised version of the Helping Alliance questionnaire. Archiv. fur Neurology und Psychiatrie 2006;157: 23-28.
32.Fenton LR, Cecero JJ, Nich C, Frankforter TL, Carrol KM. Perspective is everything. The Predictive Validity of six Working Alliance Instruments. J Psychother Pract Res 2001;10(4): 262-268.
33.Goldsmith LP, Lewis SW, Dunn G, Bentall RP. Psychological treatments for early psychosis can be beneficial or harmful, depending on the therapeutic alliance: an instrumental variable analysis. Psychological Medicine 2015;45: 2365-2373.
34.Langle A. Existenzanalyse der therapeutischen Beziehund und Sprachtherapie in Treffen. Tagungsberichte der Geseshft fur Logotherapie und Existenzanalyse 1986;2: 55-75.
***



