Somatization Disorders in Children and Adolescents – a local perspective from the Galați County
Abstract
analiza datelor calitative s-au alcatuit tabele de analiza datelor calitative s-au alcatuit tabele de contingenta calculate cu testul Chi 2 sau Testul exact al lui Fisher iar pentru datele cantitative s-a folosit Testul t test. S-a folosit un nivel de semnificatie mai mic de 0,05. Rezultate: Un total de 548 pacienți diagnosticati in perioada 1997-2003 au fost incluși. Vârsta medie a fost de 12.93+/-2.74 ani iar 69,53% au fost de sex feminin. O parte importantă din eșantion, 87,04% dintre pacienți a fost trimisi de un medic pediatru, iar în 12,96% din cazuri familia a fost cea care a solicitat consultul. Cel mai frecvent simptom la prezentare la copii a fost cefaleea. Concluzie: Abordarea multidisciplinară și complianta la tratament s-au dovedit a fi factori care prezic un rezultat pozitiv.
INTRODUCTION
Although quite common in children and adolescents, somatoform disorders have been given little attention by researchers in this population. Somatoform disorders are characterised by physical symptoms or complaints about pain that cannot be explained by a medical problem or effect of a substance. (1) Their symptoms are not intentionally produced or faked by the child and are believed to be associated with psychological factors like strong emotions or situations that threaten the individual’s physical or psychological integrity. Behavioral or emotional problems are more likely to be observed in children that exhibit psychosomatic symptoms (2).
ICD-10 subdivides these disorders into somatization disorder, undifferentiated somatoform disorder, hypochondriacally disorder, somatoform autonomic dysfunction, persistent somatoform pain disorder, and other somatoform disorders. (3) Of all these somatoform disorders, the most commonly seen in children and adolescents is persistent somatoform pain disorder. In DSM-5, somatoform disorders are called “somatic symptom and related disorders”. Somatization disorder and undifferentiated somatoform disorder from the DSM-IV-TR were combined to become somatic symptom disorder, a diagnosis which no longer requires a specific number of somatic symptoms. (4)
The prevalence of somatoform complaints in 2-17 years old population is 8-24% depending also on study design. (5-9) In a general population study, somatic complaints were found in 11% of girls, and 4% of boys. (10)
Psychosomatic symptoms in adolescents represent a transient response to stress and conflict and usually are the beginning of psychopathological conditions that can frequently lead to depression and anxiety in adulthood. Lieb and Zimmermann in 2002 concluded that somatizations are primary forms of coping strategies. (11)
Also several researchers, as Maloney in 1980 and later on, Lieb in 2007, have noted that children with somatoform symptoms are directly influenced by familial climate and they often shape their symptoms after family members or close friends. (12,13)
In children or adolescents, psychosomatic symptoms are difficult to evaluate – children are taken by their families to a specialist, in search of diagnosis and relief and are usually characterized by a lack of adherence to psychiatric medication and psychotherapy. Stigma can play a big part in this process, especially because the diagnosis of such disorders is complex as they may appear as medical conditions. Patients with these disorders typically present to general medical settings or in pediatrics departments rather than directly to mental health settings.
Another factor in the delay of evaluation and intervention for somatic disorders in pediatric population can be the lack of coherence in the multidisciplinary team that should cooperate to better solve these cases. Specialists that form these teams often do not fully understand and respect the role of the other members of the team. For example, once a child is referred to the mental health department he can still remain under symptomatic treatment in the pediatrics department, even if there is no evidence of organic disease. This attitude can make adherence to psychiatric treatment much more difficult to obtain.
The aim of this study is to get a better understanding of somatoform disorders in children and adolescents in order to be able to elaborate future guides and protocols for the assessment and treatment of this category of disorders.
MATERIALAND METHODS
A retrospective observational case series study was conducted in the Neuropsychiatry Department of „St Ioan” Emergency Hospital for Children, Galati. There were included all patients between 6 and 18 years of age that were admitted with somatic complaints not otherwise justified by a medical condition during 1997-2003. Patient records were examinated. Out of a total of 54906 patients consulted in the department in the mentioned period, a random sample of 548 have met ICD 10 criteria for D i s s o c i a t i v e d i s o r d e r , T e n s i o n h e a d a c h e , Undifferentiated somatoform disorder, Somatization disorder and were included in the study. Patients with Psychosis and/or Pervasive developmental disorders were excluded from this study. All the other subjects referred with a comorbid psychiatric diagnosis were included.
In this article, the term “somatoform symptoms” is used for somatic symptoms without underlying organic cause. The term somatoform disorders (SD) refers to the “category of disorders” according to the ICD.
Using charts abstraction the following variables were recorded: socio-demographic data (age, gender, family structure), type of consult (interdisciplinary or requested by family), clinical data (signs and symptoms at presentation, triggering or stressor factors, duration from onset of symptoms to presentation), type of treatment (specific medication, psychiatric counselling for patient and family targeting the modification of stressor conditions, symptomatic medication prescribed in Paediatrics Department) and clinical evolution. We mention that children were assessed about the presence or absence of symptoms and parents were questioned with regard to the impact of symptoms, healthcare services utilisation and past diagnoses and family history of psychiatric or neurologic disease.
Results are presented as absolute numbers and percentages. The statistical software package PASS and NCSS 2003 has been used to conduct data analysis. Contingency tables were elaborated for qualitative data and calculated using Chi-Square test or Fisher’s Exact Test. Quantitative data were analyzed using descriptive statistics and t test. The level of significance was established at 0.05 (one-tailed).
RESULTS
The mean age (+/- SD) of the admitted patients was 12.93+/-2.74 with a majority of 83,20% adolescents, aged 11 to 18 years old. Out of the total number of subjects, 381 (69.53%) were females and 167 (30.47%) were males, with 79.55% living in an urban area. More girls than boys (Female: Male=3.48:1) presented somatoform complaints in adolescence but in younger children proportions were found to be similar (Female: Male=1.36:1) and the correlation between patient’s age and sex was statistically significant (chi-square = 44.86, p< 0.01). The sample was divided in age intervals of two years. The number of female patients was higher than that of male patients in almost all age intervals with one exception, namely the interval between 6 and 8 years, where male patients exceeded female patients.
An important part of the sample was referred by a pediatrician 87.04%, whereas in 12.96% of the cases, the family was the one who asked for the consultation in the Neuropsychiatry Department.
T h e n u m b e r o f c a s e s d i a g n o s e d w i t h
Somatization Disorder was relatively constant between 1997 and 2003 with minimal variation tendencies and two lows in 1998 and 2002.
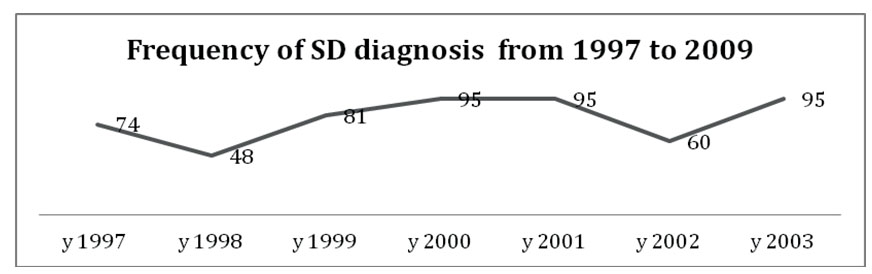
Figure 1. The frequency with which SD was diagnosed in the clinic
Female patients presented, on average, with more somatic complaints than males (n1=381, n2=167, T- test statistic= 4.96, p<0.01). A statistically relevant correlation was found between the age and the presence of pain other than headache (chi-square=15.64, p<0.01). These complaints had a peak of occurrence between 14 and 16 years of age and then abruptly dropped between 16 and 18 years. An association between gender and pain other than headache was also found, with females having these complaints more frequently (chi-square statistic =10.87, p<0.01).
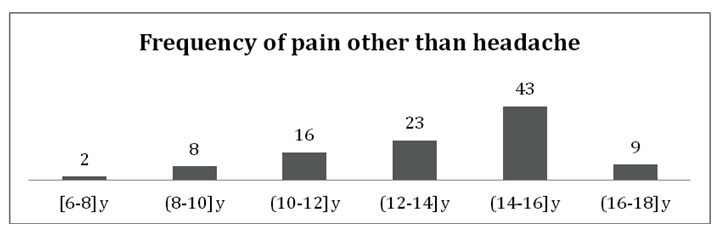
Figure 2. The correlation between pain other than headache and the age of subjects
In our sample 31.02% of the patients presented headache and this symptom was more frequent in females than in males. The correlation was statistically significant (chi-square statistic is 4.18, p=0.04). Also, cardiovascular symptomatology was more frequent in female patients (Fisher statistic=17.88, p<0.01). A similar correlation as the one found between pain other than headache and age was found for cardiovascular symptoms (chi-square statistic is 15.39, p<0.01), muscle tone modifications (chi- square statistic is 21.62, p<0.01), hypoesthesia (chi- square statistic is 17.91, p<0.01) and vertigo (chi-square statistic is 21.03, p<0.01), on one hand, and age on the other hand. These were also more frequent between 12 and
16 years and dropped in prevalence after this age.
The core symptoms (ordered by the frequency of occurance) were headache (21%), changes in muscle tone (16%), cardiovascular accuses (14%), respratory accuses (12%), pain other than headache (12%), gastrointestinal complaints (8%), and hipoesthesia (6%). Taking age into account, the second most frequent complaint after headache was gastrointestinal in young children and muscle tone modifications in adolescents (The chi-square statistic is 8.54, p<0.01). 63% of the patients were polisymptomatic, presenting with more than one of the simptoms mentioned above.
Patient history data revealed that 55.41% of the patients had parents affected by chronic illnesses. Also, ones from single parent households and those who declared tense family climate, had in average, more somatic complaints than subjects who came from harmonious family environments (single parent: T-value is 2.65, p<0.01; tense family: T-value is 2.65, p<0.01).
The most common stress factor in our lot was school pressure 50.09%, followed by living within tense families 29,62% and being exposed to a new environment
20,29%.
A statistically significant correlation was found between family condition and the persistence of somatoform complaints. Children living within tense families had, on average, a higher number of somatic complaints than those for whom the trigger was represented by school pressure (T-value is 2.36, p<0.01) or exposure to a new environment (T-value is 2.70, p<0.01). No significant correlation was found between children coming from tense families and those exposed to a new environment as far as the somatic complaints were concerned.
Considering family options, the patients followed 5 types of intervention: 32.66% received medication focused on symptoms prescribed in pediatric services, 33.58% received counseling and psychiatric treatment and 32.12% opted for both symptomatic and psychiatric treatment. A small percentage opted only for counseling 0.18% or for only psychiatric medication
1.46%. From patients treated only in the Neuropsychiatry department, 47.99% attended more than 10 sessions of psychotherapy, 38.83% required less than 10 sessions and 13.19% did not attend any psychotherapy or counseling.
Taking into account the duration of symptoms after diagnosis had been made, the sample was divided into four categories: less than 3 months (12.04%), 3-
6months (35.04%), 6-24 months (49.64%) and more than 24 months (3.28%). For children older than 10 symptoms persisted between 6 and 24 months. On the other hand, in younger children symptoms resolved from 3 to 6 months (The chi-square statistic is 21.41, p=0.04).
The clinical approach could be correlated with the persistence of symptoms. In our sample, the shortest period during which symptoms were present was reported for children with psychiatric intervention (counseling and medication). The longest period of accuses was met in patients treated entirely in pediatric clinic. Patients treated with psychotherapy and psychopharmacologic treatment had a length of symptoms after diagnosis had been made of less than 6 months. Those for whom the elected treatment was either symptomatic in a pediatrics department or combined were found to have had a longer than 6 months duration of symptoms (The chi-square statistic is 286.38, p<0.01). Studying the outcome of these patients by taking into consideration the number of symptoms (mono versus polysymptmatic), the presence or absence of chronic disease in their parents and type of family, as defined above, correlations could be established between these domains.
A longer than 6 months duration of symptoms had been found in patients exhibiting polysymptomatic accuses, as well as in those whose parents had a chronic illness (chi- square statistic is 28.05, p< 0.01). Patients coming from a harmonious family environment generally had a total duration of symptoms after diagnosis less than 6 months. As far as the rest of the patients were concerned, namely those coming from single parent families and families where tensions were reported, symptoms were found to last for more than 6 months (The chi-square statistic is 33.09, p< 0.01).
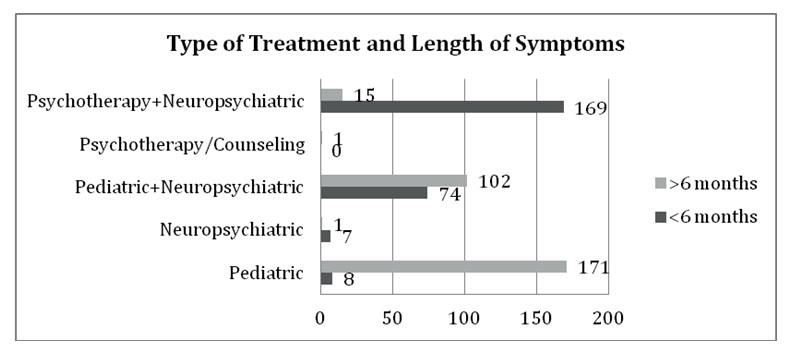
Figure 3. The correlation between the type of treatment and duration of symptoms shows better outcomes for those patients who received psychiatric care
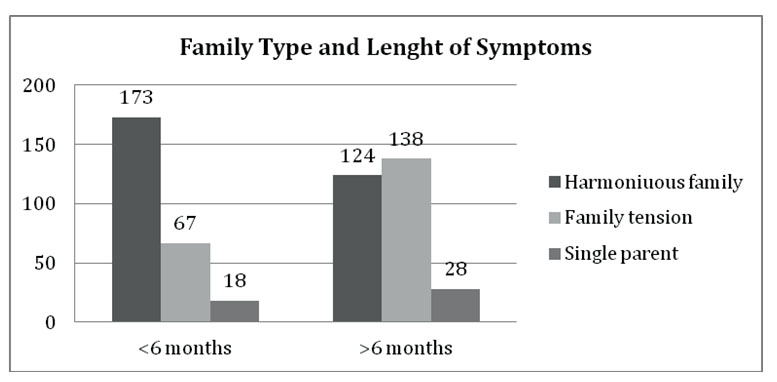
Figure 4. Correlation between family type and the duration of symptoms after the diagnosis had been made
DISCUSSIONS
The mean age and sex distribution, with the majority of patients referred for somatic symptoms being females in their teens and almost equal proportions for younger boys and girls is concordant to the findings in Campo’s study from 1999 by which he tried to classify somatic disorders in the pediatric population analyzing data from 21065 children. (14) Somatic symptoms generally occur more commonly in females than males with a ratio of 5:1, epidemiology that is similar to the gender proportion of subjects in our study. (15) It might be that a smaller sample had a little influence on the proportion found in our study (Female: Male=3.48:1), this also being the proportion found in adolescents and not all the sample. A sensibly higher number of male patients during the interval between 6 and 8 years of age, could be attributed to bigger difficulties in boys during the beginning of school that coincides with the specified age period. A 2011 report of the United States National Center for Education Statistics informs that boys are 30 percent more likely to flunk or drop out of school. (16)
The high rate of patients referred by a pediatrician (87.04%) is in total agreement with general data about somatization disorders. Presenting as organic disease, parents bring their children into mental health departments only after all objective causes for those symptoms could be ruled out.
With Romania being in a transition period from the Communist regime to a Democratic one during 1997-
2003, 1997 representing its adherence to NATO and 2004 the year when Romania became a member of de European Union, also the Mental Health System was dramatically transformed. Psychiatrists begun to use the International Classification of Disease and the growing possibility to attend international professional meetings lead to a big change in the way diagnosis was made and by this, in epidemiology. At this point we whiteness the same alarming growth in Autism Spectrum Disorders and Attention Deficit Hyperactivity Disorder as our colleagues around the world. Nevertheless, Somatoform Disorders show minimal variation tendencies.
E x i s t i n g l i t e r a t u r e r e p o r t s h e a d a c h e , gastrointestinal symptoms, musculoskeletal pain, dizziness, nausea and fatigue as most frequent accuses similarly to our findings. (8, 17) In our lot, tension headache was the most frequent symptom, although the majority of children were polisymptomatic. Our findings are consistent with data in Mohapatra’s review from 2014, which states that the prevalence of symptoms associated with somatization in the pediatric population is high, placing recurrent abdominal pain accounts for 5% of pediatric office visits on the second place after headaches that have been reported to affect 20% to 55% of all children and 10% of teenagers reporting frequent headaches, chest pain, nausea, and fatigue. (18) With 31.02% of our patients presenting with headache our data falls into the limits found by Mohapatra in general literature. We can also speculate that our finding that pain, muscle tone modifications, hypoesthesia and vertigo have a peak in occurrence around the age of 12 and 16 years old is due to the fact that between these ages children are exposed to high degrees of school and educational pressure that overlap the tense period of adolescence. This finding is also in accordance with the fact that school pressure was reported to be most common stress factor in our sample (50.09%). Pehlivanturk found 55% of the subjects in his study to have poor school performance. (19)
There had been identified the following familial risk factors as being associated with SD: somatization or organic disease of parents, psychopathology in close family members, dysfunctional family climate, traumatic experiences, and insecure attachment (20). Campo found that 40% of somatizers had psychosocial problems as coming from families with lower parental educational and/or minority background (14). In our sample children living within tense families had, on average, a higher number of somatic complaints than those for whom the trigger was represented by school pressure. Familial risk factors as single parent households, families where frequent tensions were reported, as well as parents having chronic illnesses of their own could be correlated with a longer than 6 months duration of symptoms after the diagnosis had been made. Working with children and families through counseling and psychoeducation, we are able to modify the climate, while developing abilities to express feelings and wishes.
Also, accuses persist for a longer period of time in patients showing a wider range of symptoms, which shows our findings to be similar with literature data: polysymptomatic patients have a poorer prognostic and need longer and more intensive interventions.
The study has some limitations first concerning the fact that the sample represents local experience and for sure it must be extended to presentdate. Sample representativeness has to be regarded with caution. Research on hospital samples may indicate mainly characteristics of sample selection.
Another shortcoming, found in most of similar studies is that the authors did not conduct medical examinations or if examinations were conducted, the information provided was often insufficient to judge whether it was thorough, accurate, and recent.
The retrospective nature of the study also represents one of its limits. Recall bias could have influenced the accurate recollection of actual health-care utilization, the doctor’s diagnosis, usage of medication, and determination of onset.
More research is needed to highlight the factors related to the outcome of psychosomatic complaints in children and adolescents. We consider this study a starting point for future epidemiological research in aim to get a clearer view of somatic disorders during childhood and adolescence.
CONCLUSIONS
The key in improving the outcome of children and adolescents presenting with somatoform accuses is the multidisciplinary team and a good relationship between all the team members. This collaboration between pediatric specialists and mental health services for children leads to early detection of triggers and a faster access to early specific interventions.
Although somatoform accuses are usually transitory in children, we still need some additional ways to decrease the length of symptoms in aim to:
ŘReduce stigmatization and feeling of being ill ŘIncrease good academic and social functioning ŘReduce the cost for medical services.
In this local research we found that there are
significant correlations between the duration of symptoms and family climate, clinical approach and the complexity of clinical onset manifestations.
For these children, both types of intervention, environmental – on family climate and self development, could impact the entire functioning of the future adult. That is why, early referral to mental health professionals can help avoiding unnecessary investigations and delay in diagnosis and treatment of somatoform disorders in children.
ACKNOWLEDGEMENT:
This paper is supported by the Sectorial Operational Programme Human Resources Development (SOP HRD), financed from the European Social Fund and by the Romanian Government under the contract number POSDRU/159/1.5/S/137390
References
1.Garralda ME. Unexplained physical complaints. Child Adolesc Psychiatr Clin N Am. 2010; 19(2):199209.
2.DomenechLlaberia E, Jané C, Canals J et al. Parental reports of somatic symptoms in preschool children: prevalence and associations in a Spanish sample.J Am Acad Child Adolesc Psychiatry, 2004; 43:598-604.
3.World Health Organization. Mental disorders: Glossary and guide to their classification in accordance with the Tenth Revision of the International Classification of Diseases. Geneva,Switzerland: World Health Organization, 1992.
4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edition. Washington, DC: American Psychiatric Association; 2013.
5.Berntsson LT, Köhler L. Long-term illness and psychosomatic complaints in children aged 2–17 years in the five Nordic countries. Eur J Public Health 2001;11:35–42.
6.Costello EJ, Angold A, Burns B et al. The Great Smoky Mountain Study of youth: goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 1996; 53:1129–36.
7.Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adolesc Psychiatry 1994;33:1223–35.
8.Silber TJ, Pao M. Somatization disorder in childhood. Pediatr Rev 2003;24:255–64.
9.Domènech-Llaberia E, Jané C, Canals J, Ballespí S, Esparó G, Garralda E. Parental reports of somatic symptoms in preschool children: prevalence and association in a Spanish sample. J Am Acad Child Adolesc Psychiatry 2004;43:598–604.
10.Fritz GK, Fritsch S, Hagino O. Somatoform disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:1329– 1337
11. Lieb R, Zimmermann P, Friis R, Höfler M, Tholen S, Wittchen H-U. The natural course of DSM-IV somatoform disorders and syndromes among adolescents and young adults: a prospective–longitudinal community study. Eur Psychiatry 2002;17:321–31
12. Maloney M. Diagnosing hysterical conversion reaction in children. J Pediatr 1980; 97: 1016-1020.
13. Lieb R, Meinlschmidt G, Araya R. Epidemiology of the association between somatoform disorders and anxiety and depressive disorders: an update. Psychosom Med 2007;69:860–3.
14. Campo JV, Jansen-Mc-Williams A, Comer D, Kelleher KJ. S o matization in ped iatr ic p rimary care: as s o ciation w ith psychopathology, functional impairment, and use of services. J Am Acad Child Adolesc Psychiatry 1999;9:1093–101.
15.Aro H, Taipale V. The impact of timing of puberty on psychosomatic symptoms among fourteen to sixteen year old Finnish girls. Child Development, 1987; 58: 261–268.
16.Chapman C, Laird J, Ifill N, KewalRamani A, Trends in Highschool Dropout and Completion Rates in the United States 1972-2009. U.S. Department of Education 2012-006.
17. Wolff N, Darlington A-S, Hunfeld J et al. Determinants of somatic complaints in 18-month-old children: the Generation R study. J Pediatr Psychol 2009; 1–11.. Lieb R, Zimmermann P, Friis R, Höfler M, Tholen S, Wittchen H-U. The natural course of DSM-IV somatoform disorders and syndromes among adolescents and young adults: a prospective–longitudinal community study. Eur Psychiatry 2002;17:321–31
18. Mohapatra S, Deo SJK, Satapathy A, Rath N. Somatoform Disorders in children and adolescents, German J Psychiatry 2014; 17(1): 19-24
19. Pehlivanturk B, Unal F. Conversion Disorder in children and adolescents, J Psychosom Research 2002; 52:187–191.
20. Schulte IE, Petermann F. Somatoform disorders: 30 years of debate about criteria! What about children and adolescents? J Psychosom Research 2011;70:218–228.
***




