PROTECTIVE FACTORS AGAINST SUICIDE IN PERSONS TRAUMATIZED BY ACCIDENTS
Abstract
Introducere: Evaluarea riscului de suicid după accidente, asociat cu identificarea activă a factorilor de protecție împotriva sinuciderii, poate genera strategii mai eficiente de gestionare adaptate în funcție de contexte și nevoile specifice. Obiectiv: Autorii au evaluat tendințele sinucigașe și motivele pentru a rămâne în viață după accidente de autovehicule sau de muncă - accidente legate de arsuri. Metoda: Au fost incluși 45 de pacienți de la Spitalul Clinic de Recuperare Cluj, supraviețuitorii unor astfel de accidente. Gradele de ideație suicidară și comportament suicidar dupa traumatisme și în cele 2 săptămâni înainte de evaluare au fost evaluate prin Scala de Sinucidere Paykel. Pentru a evalua factorii de protecție împotriva sinuciderii, în eșantionul studiat, a fost utilizată Scala Linehan a motivelor de viață, versiunea cu 48 itemi. Rezultate: Majoritatea pacienților incluși în studiu nu au avut ideație suicidară, planificare sau comportamente după aceste tipuri de accidente. Diferențe semnificative legate de nivelurile specifice de coping (convingerile de supraviețuire) s-au găsit între grupul cu ideație suicidară activă și ceilalți pacienți. Concluzii: Anumite motive pentru a rămâne în viață (convingeri de supraviețuire, obiecție morală la sinucidere, responsabilitate percepute de familie), pot fi considerate factori de protecție împotriva sinuciderii dupa traumatisme și pot fi benefice pentru gestionarea individualizată a traumelor pe termen scurt și pe termen lung
Assessment of suicidal ideation and behavior in persons exposed to various types of accidents is challenged by: priority of appropriate emergency medical care before any assessment of psychological needs or crisis intervention measure, heterogeneity of individual psychological response to similar types of accidents, numbers of persons affected, difficulty in following up subjects impacted by trauma (1). Insufficiently identified needs of persons traumatized by certain accidents, among which dealing with various degrees of suicidality, add to the burden of disability, negatively impact on intervention cost – effectiveness and generate mortality through suicide following trauma (2). This underlines the importance of accurate identification of subjects more prone to developing suicidality in the wake of specific types of accidents (3).
Assessment of suicidality does not generate suicidal ideation or behaviors (4); moreover, the appropriate assessment tools can identify persons and contexts in which management of suicidality needs to become a priority of posttraumatic intervention. Also, some these instruments can evaluate individual resources and vulnerabilities, which in turn can reflect in comprehensive interventions tailored to specific needs (5).
An observation derived from empirical data and supported by all current studies is that most subjects experiencing severe trauma will not actually develop suicidal ideation or behaviors (6), in spite of similarities between posttraumatic patterns of reaction (emotional constriction or numbing, perceived lack of resources, narrowed outlook about the future) (7) and common emotional and cognitive patterns associated with suicidality (hopelessness, helplessness, no escape) (8). Nevertheless, attempted and completed suicide are highly severe and entirely preventable complications in the process of psychological adjustment to traumatic events, which add to the individual and social cost of any type of trauma (9).
AIM OF THE STUDY
To assess suicidality and reasons to stay alive after trauma within a specific type of Romanian trauma population, consisting of individuals impacted by motor vehicle accidents, work – related accidents or burns, which facilitates assessment of resources and vulnerabilities related to suicidality after such traumatic events and development of effective, flexible interventions.
PARTICIPANTS AND METHOD
45 subjects treated in the Clinical Rehabilitation Hospital Cluj-Napoca – Neurology Rehabilitation Clinic (22 subjects – 48.9%) and Plastic surgery and reconstructive microsurgery Clinic (23 subjects – 51.1%) were included in the study. The following inclusion criteria were employed:
– Informed consent of the subject, approved by the Ethics Committee of the University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj-Napoca – according to the World Medical Association Declaration of Helsinki
– Exposure to trauma consisting of motor vehicle accidents, work-related accidents or burns
– The event in question endangered the subject’s life / physical integrity and/or was perceived as such by the person in the peri-traumatic context, generating a response of horror, helplessness, intense fear Data related to subjects’ gender, age, marital status, residence, date and type of trauma were assessed in the included subjects (see Table 1).
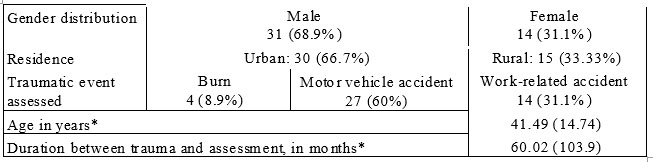
Data presented as mean (standard deviation)
Table 1. Demographic and clinical features of the studied group
The following clinical instruments were used for this study:
1.PAYKEL SUICIDE SCALE (PSS)
Paykel Suicide Scale is a 5-item versatile assessment tool, clinician-administered or self-rated, easy to employ and useful in emergency and trauma settings or clinical contexts requiring complex medical and surgical interventions (see Table 2). Incrementally increasing degrees of suicidal thought, planning and action are scored from 0 (not at all) to 5 (always) and suicide potential can thus be assessed within various timeframes and populations (10).
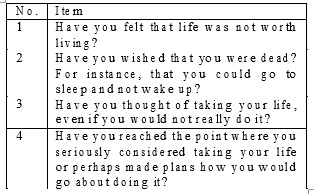
Table 2. Items of Paykel Suicide Scale
The version translated and adapted into Romanian was used for different timeframes of assessment of suicidal thoughts, plans and behaviors – the past 2 weeks, the interval between the traumatic event and the moment of assessment and lifetime.
1.LINEHAN REASONS FOR LIVING SCALE (RFL)
Linehan Reasons for Living Scale (RFL), developed in 1983, is a self-report with 48 items grouped in 6 subscales – Survival and Coping Beliefs (items 2, 3, 4,
8, 10, 12, 13, 14, 17, 19, 20, 22, 24, 25, 29, 32, 35, 36, 37,39, 40, 42, 44, 45), Responsibility to Family (items 1, 7, 9,16, 30, 47, 48), Child-related Concerns (items 11, 21, 28), Fear of Suicide (items 6, 15, 18, 26, 33, 38, 46), Fear of Social Disapproval (items 31, 41, 43), Moral Objections (items 5, 23, 27, 34). The importance of each item as a reason to stay alive is rated on a Likert scale from 1 (not at all important) to 6 (very important). This complex tool evaluates individual cognitions, beliefs and values, it is focused on the assessment of individual adjustment patterns and provides information which can further be used in developing effective, flexible and individualized prevention strategies. Both total scores, and scores for each subscale can be considered. Lack of strong reasons to live is regarded as a warning for potential future suicidal gestures (11, 12).
The 48-item version provided by the author for research purposes, translated and adapted into Romanian was used for this study. Although the scale was initially developed for suicidal subjects, the original instructions provide the possibility to employ this tool on various types of populations, exploring the reasons why the individual would not consider commiting suicide if someone else mentioned suicide as an option.
Statistical analysis was performed using Statistical Pack for Social Sciences (SPSS), Version 16.0. Mann – Whitney U test was used to assess differences in the distribution of discrete variables between two independent samples.
RESULTS
None of the 45 interviewed subjects described a suicide attempt in the 2 weeks prior to assessment. Only 2 of the 45 interviewed subjects had a history of suicide attempt; one of them described one suicide attempt prior to the referrence trauma, while the other one mentioned one suicide attempt after the referrence trauma.
The data concerning the intensity degrees of posttraumatic suicidal thoughts and plans in the studied group are presented in table 3.
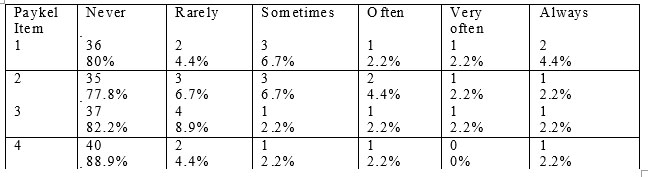
Table 3. Distribution of suicidality levels of intensity in the studied group in the interval between index trauma and assessment
The data concerning the intensity degrees of suicidal thoughts and plans in the studied group in the two weeks prior to assessment are presented in table 4.
Differences in RFL scores were comparatively assessed between the 40 included subjects who did not seriously consider or plan suicide between the moment of the accident and evaluation, and the remaining 5 who described such levels of suicidality in the aforementioned timeframe. Significantly higher scores were obtained by subjects without serious suicidal ideation or planning after trauma both for total RFL (Mann – Whitney U = 15, two- tailed p = .002), and for the Survival Coping Beliefs subscale (Mann – Whitney U = 17, two-tailed p = .003). Moreover, a comparative assessment for each RFL item revealed significantly higher scores for subjects without serious suicidal ideation or planning after trauma in 21 items of the Survival Coping Beliefs subscale (see Table
5) and in item 34 (I consider it morally wrong) from the Moral Objections subscale (Mann – Whitney U = 40.5, two-tailed p = .027).
Differences in RFL scores were comparatively assessed between the 42 included subjects who did not seriously consider or plan suicide in the 2 weeks prior to assessment, and the remaining 3 who described such levels of suicidality in the aforementioned timeframe (acute suicide risk). Significantly higher scores were obtained by subjects without serious suicidal ideation or planning in the 2 weeks prior to assessment, both for total RFL (Mann – Whitney U = 8.5, two-tailed p = .013), and for the Survival Coping Beliefs subscale (Mann – Whitney U = 17, two-tailed p = .036). Moreover, a comparative assessment for each RFL item revealed significantly higher scores for subjects without serious suicidal ideation or planning in 16 items of the Survival Coping Beliefs subscale (see Table 5) and in 2 items from the Responsibility to Family subscale: item 1 (I have a responsibility to my family – Mann – Whitney U = 22, two-tailed p = .032) and 9 (My family depends upon me and needs me – Mann – Whitney U = 11.5, two-tailed p =.009).
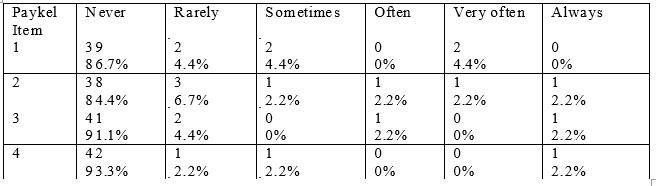
Table 4. Distribution of suicidality levels of intensity in the studied group in the 2 weeks before assessment
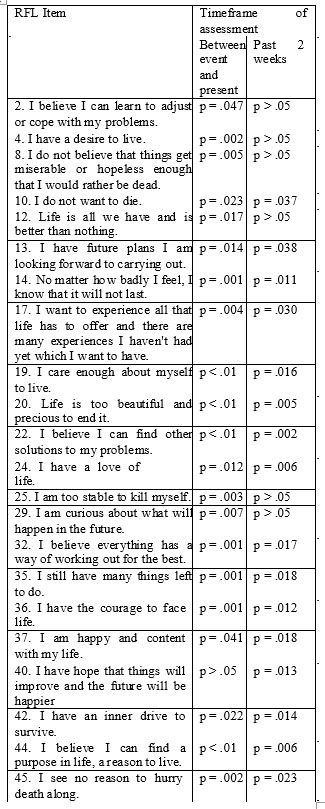
Table 5. Two-tailed p for items of the Survival Coping Beliefs subscale in which statistically significant differences were obtained in the studied samples
DISCUSSIONS
Ensuring emergency medical care and a comprehensive intervention that would prevent fatal outcomes, minimize disability and optimize interpersonal functioning is crucial after motor vehicle accidents, work- related accidents or burns (13). Nevertheless, psychological impact of such trauma is still insufficiently explored, despite both increasing awareness among medical staff in units treating exposed patients, and the positive impact of psychological intervention (when required) on overall recovery and cost-effectiveness (14).
Some authors have suggested that an illness- oriented approach to trauma in primary care may hinder posttraumatic growth and effective identification and use of resilience resources (15). Also, it has been noted that severe, pervasive disruption of posttraumatic functioning and suicide risk may be generated by symptoms that do not reach the severity of a psychiatric diagnosis (16). Nevertheless, a medical – oriented, biopsychosocial model of trauma facilitates understanding of underlying psychopathological mechanisms and intervention needs, while providing/enhancing the service network for the most appropriate assessment, referral and follow-up (17).
If suicidality in the wake of accidents is conceptualized in relationship with a specific diagnostic entity, assessment of protective factors against suicide may fall short due to a number of confounding factors, among which: diagnostic issues of posttraumatic stress d i s o r d e r a n d i t s c o – m o r b i d c o n d i t i o n s ( 1 8 ) , methodological difficulties in extrapolating the results of current studies to different populations or index events (19). Our study took these issues into account and employed a validated assessment tool based on cognitions and attitudes promoting survival and preventing suicide in all included subjects, irrespective of degree of posttraumatic symptoms ascertained.
This study is a new approach in Romanian trauma research, and the first study in Romania or elsewhere to use RFL in a specific trauma sample. The assessment of suicidality in persons traumatized by accidents, provided by the current study, confirms that active suicidal thought, planning and behaviors are rare after trauma, while adding to the still scarce and insufficient body of international data (20, 21). Thus, the current research indicates beliefs and attitudes that foster life, protect against suicide and can contribute to the improvement of trauma management strategies.By further adding a comparative sample of subjects not exposed to the types of events in question, protective and risk factors with a higher degree of specificity for these events may be ascertained. Nevertheless, the current study emphasizes the importance of self – efficacy in using internal and external resources and a pro-active outlook on life with the consequences of trauma, in order to protect against suicide in the wake of accidents such as those assessed. Data derived from this study stress that these issues are also protective factors against acute suicidality in the context of such accidents and need to be addressed in crisis interventions.
The key findings of this study prompt to specific factors related to short- and long-term intensity of active suicidal ideation and planning, which is regarded as a strong predictor of suicidal behavior in the wake of accidents (22). These factors – beliefs, attitudes, values – can be incorporated in flexible strategies that assess and address unmet posttraumatic psychological needs, target intervention to those who need it most and improve outcome.
CONCLUSIONS
1.Perceived self – efficacy and flexible, positive outlook in the wake of trauma, reflected in love and respect for life and for oneself, planning for the future, perceived courage and solutions to problems and pain, perceived satisfaction with life as it is, are identified by included subjects as protectors against suicide after the referrence accidents, both on a long-term basis, and on a shorter timeframe (the two weeks preceding assessment). The strongest protectors appear to be caring for oneself, perceived purpose, love and beauty of life, perceived alternative solutions to suicide.
2.Two types of family – related factors emerge in the studied sample as protective against acute active suicidal ideation and planning after the types of accidents assessed: the perception as having a responsibility towards the family and being needed by the family.
3.The perception of suicide as morally wrong can be used as protector against posttraumatic active suicidal ideation and planning only in longer term assessment and intervention strategies.
4.Perceived desire and curiosity to live, positive outlook on life as a whole, perceived stability and ability to cope with trauma emerged as reasons to stay alive after trauma in the studied sample on a longer term, but not in the two weeks prior to assessment. Therefore, these aspects may need to be included in short-term intervention and probably stem from posttraumatic growth.
ETHICAL CONSIDERATIONS
An informed consent, approved by the Ethics Committee of the University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj-Napoca, was signed by every participating subject – according to the World Medical Association Declaration of Helsinki.
CONFLICTS OF INTERESTS.
The authors do not have any conflicts of interests to report.
ACKNOWLEDGEMENTS.
The authors wish to thank Professor Marsha Linehan and the University of Washington Behavioral and Research Therapy Clinics, Professor Alexandru Georgescu, MD, PhD, Professor Angelo Bulboacă, MD, PhD (University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj-Napoca), Principal Psychologist
Voichița Dumitru, PhD candidate (3rd Psychiatric Clinic, Cluj County Emergency Hospital, University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj-Napoca) and undergraduate students Marius Nicula and Iulian Novac (University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj-Napoca) for their support in this research.
FUNDING SUPPORT AND ROLE OF THE FUNDING SOURCE.
The article is a part of a PhD research co-funded by the Social European Fund through the Operational Structural Programme for the Development of Human Resources (POSDRU) 2007 – 2013 „Invest in people! Doctoral Studies: through science to society”, Contract Code 6/1.5/S/3, University Babeş – Bolyai, Cluj-Napoca, Romania
REFERENCES
1.Bleich A, Baruch Y, Hirschmann S et at. Management of the suicidal patient in the era of defensive medicine: focus on suicide risk assessment
and boundaries of responsibility. Isr Med Assoc J 2011;13(11): 653-6.
2.Jurisić B, Marusic A. Suicidal ideation and behavior and some psychological correlates in physically disabled motor-vehicle accident
survivors. Crisis 2009;30(1): 34-8.
3.Clay FJ, Collie A, McClure RJ. Information interventions for recovery following vehicle-related trauma to persons of working age: a systematic
review of the literature. J Rehabil Med 2012;44(7): 521-33.
4.Mathias CW, Michael FR, Sheftall AH, Hill-Kapturczak N, Crum P, Dougherty DM. What’s the harm in asking about suicidal ideation?
Suicide Life Threat Behav 2012;42(3): 341-51.
5.Agani F, Landau J, Agani N. Community-building before, during, and after times of trauma: the application of the LINC model of community
resilience in Kosovo. Am J Orthopsychiatry 2010;80(1): 143-9.
6.Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk:
a systematic review. Arch Suicide Res 2010;14(1): 1-23.
7.Walter S, Leissner N, Jerg-Bretzke L, Hrabal V, Traue HC. Pain and emotional processing in psychological trauma. Psychiatr Danub
2010;22(3): 465-70.
8.Orbach I, Mikulincer M, Gilboa-Schechtman E, Sirota P. Mental pain and its relationship to suicidality and life meaning. Suicide Life Threat
Behav 2003;33(3): 231-41.
9.Bush NE, Skopp NA, McCann R, Luxton DD. Posttraumatic growth as protection against suicidal ideation after deployment and combat
exposure. Mil Med 2011;176(11): 1215-22.
10.Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal Feelings in the General Population: A Prevalence Study. B J Psych 1974;124: 460-
469.
11.Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you are thinking of killing yourself: The Reasons for
Living Inventory. Journal of Consulting and Clinical Psychology
1983;51(2): 276–286.
12.Ivanoff A, Jang SJ, Smyth NJ, Linehan MM. Fewer reasons for staying alive when you are thinking of killing yourself: The Brief
Reasons for Living Inventory. Journal of Psychopathology and
Behavioral Assessment 1994;16(1): 1-13.
13.Matthews L. Road trauma, PTSD and occupational functioning:
implications for policy development, intervention and rehabilitation.
Aust N Z J Public Health 1999;23(3):325-7.
14.Nickerson A, Aderka IM, Bryant RA, Hofmann SG. The Role Of
Attribution Of Trauma Responsibility In Posttraumatic Stress Disorder Following Motor Vehicle Accidents. Depress Anxiety 2012 Oct 22. [Epub ahead of print]
15.Howell A. The Demise of PTSD : From Governing through Trauma to Governing Resilience. Alternatives: Global, Local, Political
2012;37(3): 214-226.
16.Nemeroff CB, Bremner JD, Foa EB, Mayberg HS, North CS, Stein
MB. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res 2006;40(1): 1-21.
17.Konner M. Trauma, adaptation and resilience: a cross-cultural and evolutionary perspective. In: Kirmayer LJ, Lemelson R, Barad M (eds).
Understanding trauma. Integrating biological, clinical and cultural
perspectives. New York: Cambridge University Press, 2007, 300-338.
18.Benedek DM, Ursano RJ. Posttraumatic Stress Disorder: From
Phenomenology to Clinical Practice. Focus 2009;7(2): 160-175.
19.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community:
the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry 1998;55:
626–632.
20.Davydow DS, Katon WJ, Zatzick DF. Psychiatric morbidity and functional impairments in survivors of burns, traumatic injuries, and ICU
stays for other critical illnesses: a review of the literature. Int Rev
Psychiatry 2009;21(6): 531-8.
21.O’Donnell ML, Holmes AC, Creamer MC et al. The role of post- traumatic stress disorder and depression in predicting disability after
injury. MJA 2009;190: S71–S74.
22.Simon RI. Suicide risk assessment: What is the standard of care?
Journal of the American Academy of Psychiatry and the Law 2002;30(3):
340-344.
***




