THE OBSESSIVE COMPULSIVE AND RELATED DISORDERS IN DSM V. NOVELTIES AND CHALLENGES
Abstract
Capitolul privitor la Tulburarea Obsesiv-Compulsivã ºi Tulburãrile Corelate este unul nou în DSM V. Modul de abordare este cel al spectrelor maladive. Capitolul exprimã opinia specialiºtilor în domeniu, dar nu sugereazã argumentele care au determinat includerea în acelaºi capitol a unei colecþii de tulburãri care nu întotdeauna apar ca evident corelate. Propunerea fãcutã de DSM V invitã la dezvoltarea unor modele teoretice ºi doctrinare care sã clarifice aceastã problemã. Funcþiile cognitive ale „coerenþei centrale” (1, 2), cele executive ºi doctrina evoluþionistã ar putea fi utile în acest domeniu.
The Obsessive-Compulsive Disorder (OCD) is presented in DSM V (1) in a new chapter, different than the one of the Anxiety Disorders, as it used to be in DSM IV TR (2), named “Obsessive-Compulsive and Related Disorders”. It is an option that places the manual closer to the perspective of ICD 10 (WHO) (3). Besides the Obsessive-Compulsive Disorder, the chapter includes: the Body Dysmorphic Disorder, the Hoarding Disorder, Trichotillomania, the Excoriation (Skin-Picking) Disorder, Substance/Medication-Induced Obsessive- Compulsive and Related Disorders and Obsessive- Compulsive and Related Disorder Due to Another Medical Condition.
The structure of the OCD chapter reveals the spectrum perspective. This perspective, the developmental approach and the similarities with the ICD-10’s structure are the main novelties of the DSM V. The clinical psychopathology of the last 20 years has focused on the idea of the spectrum. This perspective has been used not only for the Obsessive-Compulsive Disorder (4), but also for the bipolar disorder, schizophrenia, autism and other disorders (5). In DSM V, it is sometimes mentioned in the titles of the chapters (e.g. Schizophrenia Spectrum and Other Psychotic Disorders), in the name of the disorders (e.g. Autism Spectrum Disorder) or it is inherent thorough the grouping and the way of presentation of the disorders in a certain chapter, by using the expression “Related Disorders” (e.g. Bipolar and Related Disorders). The chapter regarding the obsessive-compulsive disorder is part of this last category, though it has some particular characteristics.
The OCD spectrum, as it is presented in DSM V and other monographies (6) is different from Hollander’s version, which focused on the continuum between different psychiatric disorders. The current concept of the spectrum sustains the continuity between clinical, subclinical manifestations, temperament and the bio- psychological vulnerability of the patient and his first degree relatives (7).
Hollander described three psychopathological axes. One of them is expanding from the pole of the obsessive-compulsive indecision to the incontrollable impulsivity. It includes different entities:
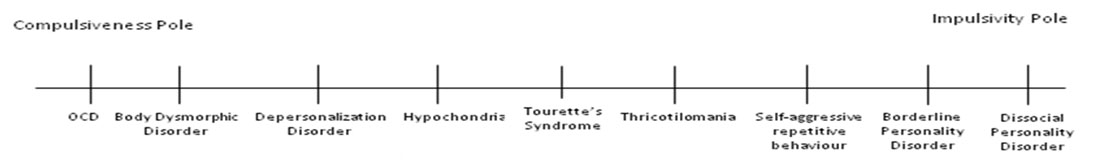
DSM V does not accept this vision and there is no c o m m e n t r e g a r d i n g t h e t r a n s i t i o n b e t w e e n compulsiveness and impulsivity in the manual.
The second axis in Hollander’s system is the one between the obsessive self-control of the movements and the involuntary movements, not only tics, but also the extrapiramydal ones. This idea is justified by the discovery of OC symptoms secondary to Huntington’s chorea, leading to important research regarding the dysfunction of the basal ganglia in OCD (8). DSM V describes a form of OCD associated with tics, with a poor prognosis, but it makes no further comment on this subject. Likewise, there is no comment in DSM V regarding the interference between the Tics Disorder (Gilles de la Tourette), in which the obsessive symptoms are present in 30-50% of the cases, and OCD.
The last axis described by Hollander refers to the transition between the uncertainty in OCD and the delusional certainty.
Taking into consideration these aspects, the following question arises: what is the argument based on which DSM V classifies the disorders in the chapter “Obsessive-Compulsive and Related Disorders”? There is no explicit answer to this question, neither in the manual, nor in other published reviews (9). Still, we can understand it better if we consider the basic groups of symptoms in OCD described in the meta-analyses on this subject more than a decade ago (10,11). These are: – contamination/washing/cleaning; – preoccupation for order/symmetry, counting; – harm obsessions with checking compulsions; – hoarding. The DSM V maintains this classification, but places the Hoarding Disorder in a separate class. We will try to reason the fact that the specificity of these symptoms supports the grouping of the disorders in the same class.
Thricotilomania and the Excoriation (Skin- Picking) Disorder express an exaggerated preoccupation regarding the subject’s own body, which is similar to the obsessions from the contamination/washing class. The focus on the details and the repetitive, quasi-stereotyped movements are other common features of these categories. Still, the idea of contamination can have a prevalent and even delusional intensity when the insight is lost. In order to have a more specific framework for the OCD pathology, a comparison with the schizophrenia spectrum could be useful.
In the paranoid delusions, the subject is convinced of the fact that other persons want to harm him. In OCD, the subject does not believe that the danger comes from other persons, but from invisible agents, such as germs and dirt. Alternatively, in one of the OCD subclasses, the subject obsessively experiences the intention of harming other persons, for example of hitting people or killing his own child. By the means of the psychopathological phenomenon called the “thought- action fusion”, the subject believes that, for example, by thinking that his wife could have an accident, he can really produce that accident. These delusional experiences are part of the more severe forms of OCD, in which there is no insight. However, it is not the delusion that is specific for OCD, but the area of preoccupations that characterizes this class of disorders: the preoccupation for the vulnerability of one’s body and the aggressive intentions towards other people.
Another specific aspect of OCD is the preoccupation for order and symmetry, for arranging the spatial environment so that “everything is in the right place”. This theme is correlated with the exaggerated focus on details. Together with hoarding, it reveals the impairment of a function (also present in Kanner’s autism), called by Uta Frith “the central coherence function” and by Baron-Cohen “the systematising” function.
Finally, we need to mention the Hoarding Disorder. Although it has been described as a subtype of the OCD in the last decades, hoarding is mainly a characteristic of the Obsessive-Compulsive Personality Disorder (OCPD) and it is still mentioned in DSM V at the OCPD. Why was it included as a separate category in the DSM V? Maybe because of its high frequency in the overcrowded cities of the occidental world. Hoarding has always been described, all over the world, as a normal personality trait. But it is also correlated with other i m p o r t a n t p e r s o n a l i t y f e a t u r e s : t h e n e e d f o r systematisation and hierarchical classification. As part of the OCD symptomatology, hoarding would be similar to the obsessions for order and ordering. As a psychic trait, from Baron Cohen’s perspective, it would be complementary to empathy, a function which is especially impaired in autism. Considering these correlations, t a connection between OCD, OCPD, OCD spectrum and the autism spectrum can be revealed (12).
Another question to be answered would be: How comes that OCD is characterized by such diverse themes of the obsessive experiences (contamination, order, aggressive intentions)? And what is the correlation between OCD and OCPD? That is because, statistically, OCPD is not strongly correlated with OCD. We could understand this problem if we take into consideration the role of the executive functions. A common aspect of all these themes is the impairment in the performance of an action which the subject needs to accomplish by using his own body. When performing an activity, he is following a specific order towards a purpose and he is permanently evaluating and controlling his actions. This problem needs a special analysis, because it emphasizes the correlation between the obsessive-compulsive disorder, autism and disorganized schizophrenia. If we only consider their symptoms, schizophrenia and OCD seem distinctive entities, as suggested by Poyurovsky’s recent monography (13). Still, from the perspective of the executive functions’ impairment and the similarities with the autism disorder, some useful models of interpretation for the future studies can be developed (14).
CONCLUSION
DSM V’s approach of the Obsessive-Compulsive and Related Disorder is a demanding novelty. The grouping of the disorders in this chapter is based on the spectrum perspective and it leads to cultural evolutionary interpretations (which were not discussed in this paper). This approach challenges the researchers to develop theoretical models that can explain this classification and that can be later tested.
REFERENCES
1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Washington, DC: American Psychiatric Publishing, 2013.
2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edn, Text Revision. Washington, DC: American American PsychiatricAssociation. 2000.
3.World Health Organization, The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines.Geneva: World Health Organization, 1992.
4.Ho11ander E, Wong CM. Obsessive-compulsive related disorders. Washington:American Psychiatric Press, 1993.
5.La.zarcscu M. Spcct:rul schi?.ofrcn. Psikiatru.ro 2008;27: 18-25.
6.St:eketee G (ed). The Oiford Handbook of Obsessive Compulsive and Spectrum Disorders.Oxford University Press, 2012.
7.La.zarescu M. Noile frontiere ale nosologiei. Psihiatlu.ro 2010;23: 24- 27.
S.Bouvard M. Lea troubles onsessWnnels compulsives. Paris: Masson, 2003.
9.0bsessive-Compulsive Spectrum Disorders. Dialogues in clinical neuroscience2010; 12(2).www.dialogue!H:tlli.org.
10.Mataix..C01s D. ct al. Relation of factor-analyzed symptom dimensions of obsessivemcompulsive disorder to personality disorders.
ActaPsychiatrica Scrmdinavica2000; 102: 199-200.
ll.Leckman JF. Symptoms of obsessive compulsive disorder.American Journal ofPsychiatry2005;154: 911-917.
12.Uz!i:rescu M, Bumbea 0. Patologie obsesiva. Bucuresti: Ed. Academiei Romarte, 2008.
13.Poyurovsk:y M. Schizo-Obsessive Disorder. Cambridge University Press,2013.
14.Lazarescu M. Bazele Psihopatologiei Clinice. Bucuresti: Ed. Academiei Rom.ane, 2010.
……




