PERSONALITY DISORDERS AND PSYCHOTIC DISORDERS – CO-MORBIDITY IN FORENSIC INPATIENTS
Abstract
Introducere: Tulburarea de personalitate comorbidă cu tulburarea psihotică reprezintă o provocare permanentă în practica zilnică. Scopul acestui studiu este de a analiza implicațiile diagnosticului dual de tulburare psihotică și tulburare de personalitate la pacienții internați pentru aplicarea măsurii de siguranță. Metodă: Este un studiu non-intervențional realizat în SPMS Săpoca pe durata unui an. Pacienții diagnosticați cu schizofrenie sau altă tulburare psihotică, internați asistați cu măsură de siguranță au fost evaluați pentru diagnosticarea unei tulburări de personalitate. Am colectat date socio-demografic și antecedentele psihiatrice, pernal și am urmărit pe durata studiului: tratamenul farmacologic, participarea la terapia ocupațională și comportamenul violent. Au fost folosite instrumente de evaluare a psihopatologiei (PANSS,CGI) și a riscului de violență (HCR-20) inițial, la 6 și la 12 luni. Analiza statistică s-a realizat cu SPSS 17.0. Tratamentul a fost decis de medicul curant în cel mai bun interes al pacientului. Am folosit numai informații din documentele medicale. Designul studiului a fost aprobat de Consiliul Etic al SPMS Săpoca. Rezultate: Din eșantionul de 128 de subiecți 50,7% au fost diagnosticați cu o tulburare de personalitate, cel mai f re c v e n t a n t i s o c i a l ă ( 3 6 , 9 % ) . E x i s t ă c o re l a ț i i semnificative între tulburarea de personalitate și consumul de alcool, slaba participare la terapia ocupațională, apariția violenței. Eșantionul a fost împărțit în două loturi: cu și fără tulburare de personalitate. Testul Mann-Whitney a confirmat corelațiile obținute prin crosstabulare. Între loturi au existat diferențe privind ameliorarea(ANOVA mixt): PANSS-T (p=0,032), CGI-S (p=0,007 și apariția violenței (analiza Kaplan- Meyer:Log Rank=16,177, p =.000). Concluzii: Tulburarea de personalitate, cel mai frecvent din clusterul B,comorbidă tulburării psihotice, este destul de comună în acest eșantion de pacienți forensic și este asociată independent cu un risc crescut de violență în psihoză. Această observație este importantă pentru evaluarea și managementul riscului la pacienții internați pentru aplicarea măsurii de siguranță. Studii ulterioare sunt necesare având în vedere limitele metodologice.
INTRODUCTION
Personality disorders (PDs) are common, debilitating psychiatric conditions that have enormous costs to patients and their family members, and more broadly, to society. Unfortunately, these conditions are also widely misunderstood and misdiagnosed (1). With respect to prognosis, PD may be associated with increased risk for criminal and violent behaviour, as well as with poor response to psychosocial rehabilitation and crime reduction programs (2). More than half of those with PD also had an axis 1 disorder (3) and patients with co-morbid psychotic disorders and personality disorders are among the heaviest users of psychiatric services (4) and forensic services also. On the other hand, the number of forensic psychiatric inpatients has been growing markedly and risk assessment and management of patients with severe mental illness are increasing priorities for mental health services (5).
There is few data in literature relating to those with schizophrenia (or other schizophrenia spectrum disorder) also diagnosed with personality disorder who committed a criminal act (more often violent) and are referred to forensic psychiatric services (compulsory hospitalization as medical safety measures according Romanian law).
The primary objective of this study is to analyze the implications of PD co-morbid with schizophrenia (or other schizophrenia spectrum disorder) on the clinical course and treatment received and on violent behaviour in patients admitted to implement safety measures of a medical nature. The secondary objective is to provide epidemiological data essential for the development of forensic mental health services strategy.
MATERIAL AND METHOD
Participants. Procedure
The study is a longitudinal and observational,non-interventional one, accomplished by Sapoca PSMH (Psychiatry and Safety Measures Hospital) during 12 months in 2008-2009. There were included in the study patients hospitalized in forensic psychiatric wards diagnosed with schizophrenia or other schizophrenia spectrum disorder: F20-F29 according to ICD 10 (International Classification and Statistics of Diseases and Related Health Problems, Revision 10), aged 18-65 years who have signed consent for participation. There were excluded patients with length of stay longer than 2 years. The baseline data were obtained from medical and legal documents. Patients were evaluated and have been applied scales: SCID-II (Structured Clinical Interview for Personality Disorders Clinical), PANSS (Positive and Negative Symptom Scale – Scale of positive and negative symptoms in schizophrenia), CGI-S (Clinical Global Impression – Clinical Global Impression -severity) and HCR-20 (Historical Clinical and Risk Management). Information used was: socio-demographic data (age, gender, origin, education, and occupation), psychiatric, forensic and criminal history, alcohol use, offense. The patients were evaluated at baseline, at 6 months and 12 months (end of study): PANSS, CGI-S, and HCR-20.
During the study period we followed the therapeutic plan (antipsychotics, mood stabilizers, and occupational therapy – OT) and the interpersonal violent behaviour.
Instruments
Psychotic disorder was diagnosed accordingly to ICD-10 (6) and PD was assessed with semi-structured interview SCID-II (7) only from a categorical perspective and not dimensional and the diagnosis was based on ICD-
10 (F60-F61). To evaluate the clinical course we used PANSS (positive, negative, general and total scores, excited- component score) and CGI-S (8, 9).
To assess the risk of violence it was used HCR-20, scores (subscales: H, C, R and total) and violence risk assessed (low, medium and high). The final risk assessment of violence was made following the discussions of the two independent assessors with accredited training (10). The HCR-20 was used only for research purposes and the proposal to change the safety measure by the forensic psychiatric commission being based on the current methodology (mainly clinical judgment).
Violence in hospital was considered only if it had been documented by medical staff and it was understood as damaging to one or more persons that an attempt or threat as described by the authors of the HCR-20 (10). Statistical analysis of data was performed with SPSS 21.0. (Statistical Package for Social Sciences) for Windows. The tests used were chosen based on the type of variables: t test for two independent samples (interval variables), chi- square test of association – cross-tabulation (for nominal and ordinal variables), correlational analysis, Mann- Whitney test, ANOVA test (repeated measures, mixed), Kaplan-Meyer survival analysis.
Ethical Considerations
The study was non-interventional, data used were collected only from medical and forensic records and the three assessments of the study corresponded to periodic assessments of forensic inpatients according to the law. The therapeutic program was conducted by the treating psychiatrist in the patient’s best interest. Methodology of the study and informed consent model were approved by Ethical Board of Sapoca PSMH. Throughout the study it was considered legal and privacy rights of the volunteer participants. The study was conducted on a vulnerable population.
Methodological limitations
There are considered as methodological limitations: the small number of participants and the lack of validation on Romanian population of assessment tools used. Evaluation of violent behaviour and participation in occupational therapy (OT) based on the information noted in the observation sheets by untrained medical personnel specifically for the study.
RESULTS Participants
At screening the group of 128 subjects were
diagnosed with schizophrenia or other schizophrenia spectrum disorder and 28 of them had a diagnosis of PD. At baseline assessment there were identified 65 subjects with PD and 63 without PD. 109 subjects completed the study (53 with PD and 56 without PD); the reasons for non-completion (19 cases) were different (medical, legal, withdrawal of consent, unauthorized leaving hospital) (Table no.1).
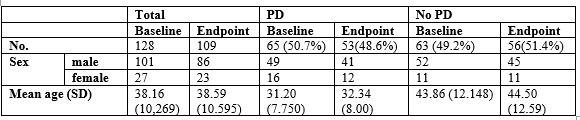
Table 1. Group and subgroups: distribution on sex and mean age
At baseline the most commonly diagnosed was antisocial PD (36.9%) followed by borderline PD and mixed PD, noting important differences towards screening (diagnosis established by initial forensic expertise) (Table no.2).
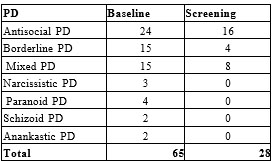
Table2. Type of PD’s – baseline vs. screening
We observe dominant PDs from the B cluster (antisocial, borderline, narcissistic – 64.6%) while the PDs from A cluster (paranoid, schizoid, schizotypal) represents 9.2% and C cluster (anankastic, dependent, avoidant) only 3% (Figure 1).
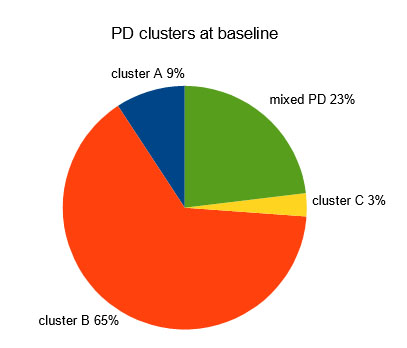
Figure 1. A pie-chart illustrating the distribution of PD
clusters at baseline
Comparative presentation of lots (PD vs. no PD)
The two samples were analyzed by independent t-test (age, scores, length of stay) and chi-square test (sex, occupation, education, area of origin, marital status, alcohol use, psychiatric, forensic and criminal history, violence risk). Subjects with PD were younger than those without PD, the mean age was lower in the PD group with statistical significance: t (104.7) = – 7.003, p = .000.
Groups are similar in terms of psychopathology and clinical symptoms, that there were no significant differences (p>0.05) for all the scales and subscales scores obtained (PANSS, CGI, HCR-20). PD significantly correlated with the risk of violence assessed at baseline: χ2 (2) = 7.81, p = 0.02. PD is associated with alcohol consumption: χ2 (1) = 37.611, p = 0.000, phi coefficient =
0.542, the relationship between the two variables is strong (according to Cohen, 1988); likehood of alcohol use (OR) is 12.5 times higher in PD group than no PD group (95% CI, 5.2-30.2) (Figure no. 2).
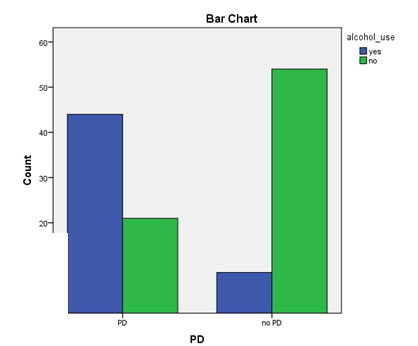
Figure 2. The relationship between PD and alcohol use for final sample
PD significantly associated with criminal records: χ2 (1) = 28.646, p = 0.000 and forensic history: χ2 (1) = 38.763, p = 0.000. PD is not significantly statistically associated with: gender, rural origin, marital status, occupation, education and psychiatric history (p>0.05).
In the group with PD violent index offenses are more common than in the group without PD (45 vs. 34) but the difference is not statistically significant (p = 0.116). Murder is more common in the group without PD (21 vs.15) also without statistical significance (p = 0.358). PD type mattered, with statistically significance (Kendall tau_b correlation), for criminal records (0.447, p = 0.000) and for participation in occupational therapy (-0.228, p =
0.047) and for repeated violence (0.371, p = 0.001). From the descriptive analysis it was observed that patients with antisocial PD often had a criminal history and those with borderline PD paticipated less at occupational therapy. Repeated violence during the study was more common those with antisocial PD and mixed PD. There were no statistically significant correlations between types of PD and other variables.
The clinical course
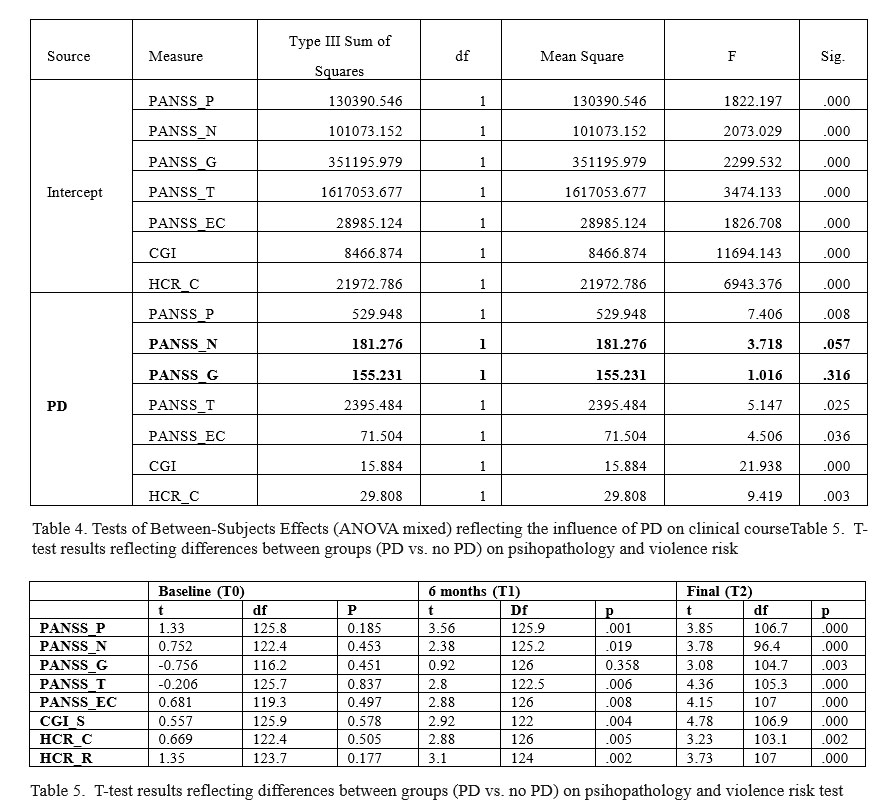
In both groups (with and without PD), clinical improvement was statistically significant (p=0.000, ANOVA test combined), for all scores, at 6 months and 12 months also. The improvement between baseline and endpoint differ significantly between groups (with and without PD) according the effect of interaction time*PD, this means the improvement is significantly better in the group without TP (Table no. 3). Table no. 4 (Tests of Between-Subjects Effects) show that the main effect of PD is statistically significant for all scores, except PANSS_N (negative) and PANSS_G (general).
Clinical improvement is significant for the first six months of the study (0-6 months) for all scores while, in the second period of 6 months (6-12 months),improvement is only significant for PANSS_N, PANSS_G, PANSS_EC, and PANSS_T. There is no significance for PANSS_P, CGI-S, HCR_C, and HCR_C. Post-hoc tests confirm the statistic significance presented. At the independent t test was significant difference (p
<0.05) between the two groups for all scores followed, both at 6 months and at endpoint (Table no. 5).
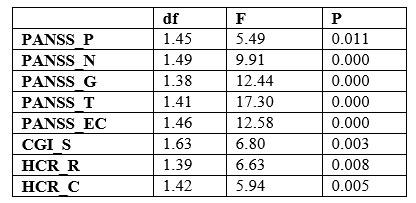
Table3. Results to ANOVA repetead measures
Violent behaviour
PD significantly correlated with violence (Pearson correlation): 0.415, p=.000 and there were statistically significant differences between the 2 groups on violent behaviour during the study: χ2 (1) =22.056, p =
0.000 (Figure 3). Observations were confirmed by
Kaplan-Meier survival analysis: Log Rank = 16.177, p =
.000 (table no.6) Patients with PD had a seven times higher risk of having a hospital violent behaviour (OR = 7.35,
95% CI, 3.02-17.90) (Figure 4).
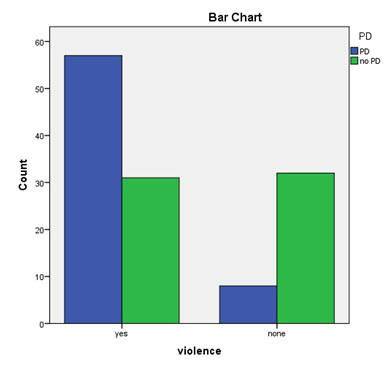
Figure 3. A bar chart reflecting relationship between PD
and hospital violent behaviour
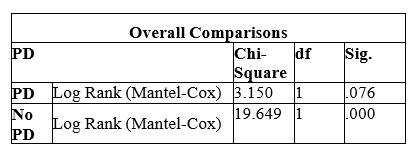
Table 6. Results of Kaplan Meyer Analyse reflecting occurence of violence
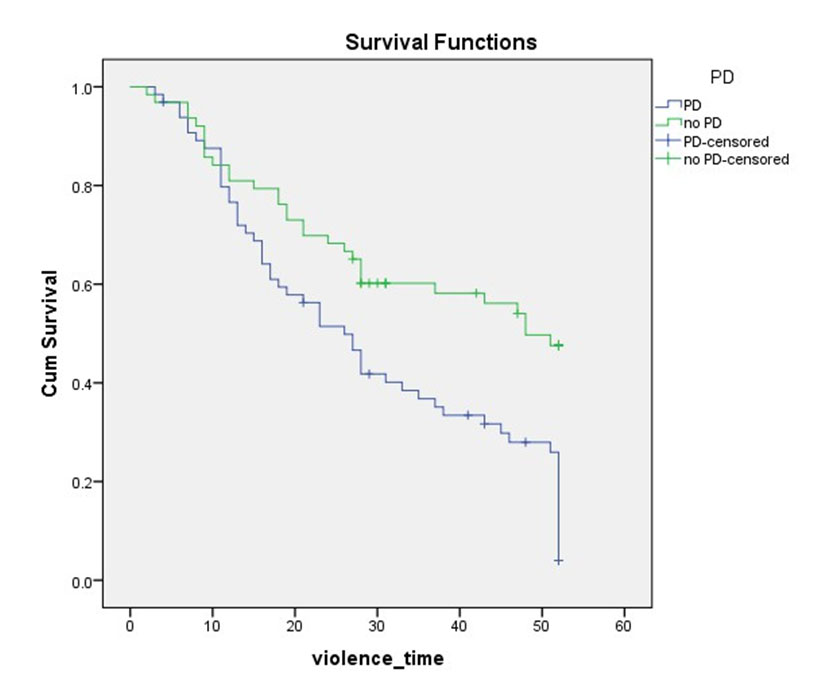
Figure 4. Kaplan Meier survival analysis demonstrated poorer survival (no violence) in PD group
PD correlated significantly with repeated violence: χ2 (1) = 10.743, p = 0.001; those with PD have a 3.5 times higher risk for repeated violence (OR=3.5, 95% CI, 1.63-7.62)
Treatment plan
There were statistically significant differences between groups regarding the therapeutic plan (chi-square test). PD significantly correlated with: the use of antipsychotics in combination, the use of mood stabilizers and low participation in OT (table no. 7).
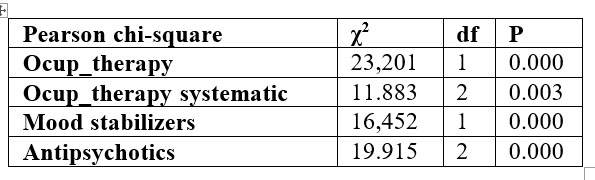
Table 7. Differences on treatment plan
Participation in OT is negatively correlated with violence, which means that participation in OT can be considered protective factor for the occurrence of violence only in the group without PD. Only in the group without PD, chi-square test showed a statistical significance between participation in OT and violent behaviour: χ2(1)
= 12.270, p = 0.000, an observation confirmed by Kaplan- Meyer survival analysis.
In the group without PD, participation in OT is an independent factor with statistical significance to clinical improvement in subscales: PANSS_ P (p = 0.002), HCR_R (p = 0.000) and HCR_C (p = 0.000), but in the group without co-morbid PD, participation in OT does not correlate with clinical improvement than for HCR_C (p = 0.024). Note that patients with schizophrenia and PD participating in OT have a better evolution in terms of positive symptoms and risk factors. PD correlates with poor therapeutic compliance and even with therapeutic resistance. Therapeutic compliance is seen better by participating in OT because pharmacological treatment administration is strictly monitored by medical staff.
Patients with psychosis and co-morbid PD were more often treated with a combination of antipsychotics than with monotherapy but without statistical significance. Type of antipsychotic drug used (first generation, second generation, combination) does not matter in clinical outcome for patients regardless of the presence of PD. These results are confirmed in mixed ANOVA: there is interaction effect, time*antipsychotics, only for PANSS_EC (p=.012) and only for psychotic PD patients. There isn’t any interaction effect with statistical significance in the group without PD. Significant difference was observed only for PANSS-EC subscale (p = 0.000) in the PD group which means that the use of antipsychotics in combination was an independent factor for decrease PANSS-EC score. This observation supports the complexity of therapy necessary for these patients (PD co-morbid schizophrenia) with the rising cost of hospitalization.
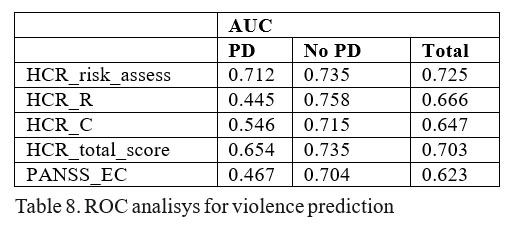
Risk assessment
PD mattered significantly for the discharge proposal: χ2(1)=7.07, p=.008. Patients without PD had a higher likelihood (OR=3.3, 95% CI, 1.33-8.23) of being proposed for discharge compared to those with PD co-morbid schizophrenia.
There was a statistically significant correlation between the PD and HCR-20 risk-assessed (low, medium, high): χ2 (2) = 7.81, p = 0.02.
In terms of predictive validity for violent behaviour we analyzed HCR-20 risk assessed, HCR-20 scores (total, C, R), PANSS_EC and observed an average predictivity (0.7 to 0.75) for the group without PD and a low predictivity for the group with PD (table no.8).
DISCUSSION
The first observation is related to under- diagnosis of PD in forensic practice: only 28 (21.8%) subjects were diagnosed with PD (generally antisocial PD
– 16) co-morbid schizophrenia (or other schizophrenia spectrum disorder) compared to 65 (50.7%) diagnosed at screening. In 5 cases it was diagnosed another type of PD. Regarding the diagnosis of schizophrenia (or other schizophrenia spectrum disorder) there were only 22 cases where the screening diagnosis was different, but in the same spectrum: F20-F29.
Epidemiological data obtained correspond to the literature regarding prevalence PD and co-morbidity with psychotic disorders and prevalence of cluster B PD (antisocial, borderline, histrionic, and narcissistic) but also in terms of: gender, average age, alcohol consumption. Review of the literature reveals limitations in comparing results among previous studies about PD, possibly due to variability in the types of populations, measures, and patterns of analysis. This was demonstrated by widely differing prevalence rates of personality disorders (11).
In sharp contrast to our results, a large proportion of patients in Dutch forensic hospitals have a PD without a concomitant major mental disorder (12) but, the same, cluster B PD is predominant: in a sample of 94 patients,
66% fulfilled diagnostic criteria for a cluster B (13). In other sample of 39 patients: 87 % received a diagnosis of PD, most often from cluster B (14). In a German forensic sample (141), 51 have one PD and only 18 have psychosis and more than half of the patients have had a drug or alcohol problem (15). In a sample of 162 forensic in- patients from the same Romanian Forensic Hospital (PSMH Sapoca), 58 (36%) were found with one PD and
39 (24%) were diagnosed with schizophrenia and co- morbid PD (16).
In secure hospitals from UK: 88% are men, mean age was 37, 86% had schizophrenia and 85% had problematic use of alcohol ( medium security unit) and mean age was 40 years, 61% had schizophrenia, 45% PD and 10% are dually classified (high security unit) (17). Mean age (31.2 years) was similar with those of Romanian forensic sample (35.2 years) (16) and German forensic patients (36.5 years) (15).
There are few data about offenses: patients from German sample have different crime backgrounds (54% sexual offenders, 27% battery or murder) (15) and in UK medium secure unit: 25% murder/attempting murder, 29% wounding, 20% assault and 10% sexual offence (17). In our study, violent offence was more frequent in group with schizophrenia and co-morbid PD (69%) than without PD (54%) and it is remarkable the absence of sexual offenders in our sample, probably because of the lack of victim’s courage to recognize their problem.
Alcohol consumption is frequently associated with PD and schizophrenia and it is an independent risk factor for violence seen in the literature data. There is an association of homicide with mental disorder, particularly with schizophrenia, antisocial personality disorder and drug or alcohol abuse (18). Cluster B PD is, undoubtedly, the most related to criminal and it is the most connected to alcohol/drug abuse, which is a clearly precipitating factor of violence (19) and antisocial PD is a risk factor for developing problem drinking and often antisocial PD develops a few years before the drinking (20).
Mihailescu and Mihailescu, 2007 (21) showed that marital status, alcohol abuse, previous psychiatric hospitalizations were predictors of violent behaviour in schizophrenia (21).
PD co-morbid schizophrenia was associated with an increased risk for violence and a more complex treatment. PD relationship with violence is complex because of the variety of PD, high co-morbidities and the difficulty of establishing causality (22). Personality dysfunction is often a co-morbid condition, making it difficult to determine direct causation. Although co- m o r b i d i t y a s a c l i n i c a l c o n c e p t c a n i n c r e a s e understanding, in the legal arena it can lead to confusion by making apportionment of responsibility or fault more difficult (23).
Co-morbid PD are also likely to be independent risk factors for violence in individuals with schizophrenia (24,25) and personality pathology can be a significant predictor of aggression in patients with schizophrenia (26). The risk of violence in patients with schizophrenia is significantly increased by association with antisocial PD and borderline PD (27) and co-occurrence of schizophrenia and borderline PD is not infrequent and that borderline PD has a significant negative longitudinal impact on the course and outcome of patients with schizophrenia (28). In most respects, offenders with schizophrenia and high levels of psychopathic traits seem to be similar to psychopathic offenders without psychotic illness, which has implications for early intervention and management (29). Co-morbidities are frequently implicated in violent behaviour of psychotic patients, and their detection and treatment are therefore of primary importance. Psychosocial treatments are necessary components of the management of violence in psychosis (30).
Better predictivity in schizophrenic group without PD raises questions considering that psychopathy is an H subscale factor (HCR-20) and, the same, the differences from international observations on the HCR- 20 violence predictivity (10) but can be explained by methodological limitations of the study. PD correlates with more frequent use of combination of antipsychotics and mood stabilizers and low participation in occupational therapy which resulted in a limited clinical improvement for those with PD and schizophrenia. Non-completion of treatment of PD has been associated with a number of negative consequences, including retention of criminal attitudes (31), poor global functioning and higher rates of hospitalization (32). Evidence of effective therapeutic programs for PD is limited especially regarding long-term outcomes (including antisocial behaviour): cognitive- behavioural interventions have the best evidence base and pharmacological interventions using mood stabilizers and atypical antipsychotics may be effective for some symptoms of personality disorders (33). In addition to relapse prevention and psychiatric symptom relief, the benefits of antipsychotics and mood stabilisers might also include reductions in the rates of violent crime (34). There are 3 inevitable problems related to treatment of violent patients with PD: PD are egosyntonic and PD patients not accessing psychiatric services only in cases of emergency/crisis or when associated another mental disorder (35).
The Dutch forensic mental health field focus on treatment of dynamic risk factors for new offenses, of which PD is one (12) and the UK is recognising the importance of mental health awareness and reduction of stigma, and has begun to integrate access to treatments with employment services (36).
All these issues outline wavy evolution marked by non-compliance and treatment resistance. These problems lead to prolongation of hospitalization and to increased costs during hospitalization. In this context, we believe that assessment and accurate diagnosis as both a psychotic disorder and a co-morbid personality disorder it would facilitate access to complex individualized treatment programs. Best specialized mental health services for people with PD and schizophrenia may be provided in specific treatment units for PD patients. The literature discussing where forensic patients with PD can be treated: forensic hospitals or prisons (17).
PD people are heterogeneous in terms of variety, consistency and intensity of their symptoms (35), problem whose solution is tried with categorical and dimensional hybrid model proposed by DSM 5. The new model contribute to greater understanding of the causes and treatments of personality disorders and, as clinicians become more familiar with the new PD model, patients are likely to receive more accurate assessments and diagnoses, leading to improved clinical care (1).
CONCLUSIONS
The study achieved its primary objective of identifying the implications of PD co-morbid with schizophrenia (or other schizophrenia spectrum disorders) on forensic patients: PD is associated with alcohol use, violent behaviour and the need for complex and individualized therapeutic programs. These observations are important for assessing and managing violence risk in hospitalized patients assisted with medical safety measures (forensic patients). The survey data showed that PD co-morbidity is common in schizophrenia and most often is a cluster B PD and thus was fulfilled and the secondary endpoint to provide epidemiological data necessary development strategies forensic mental health services. Given the ethical and legal implications of judicial psychiatry is vital to providing quality services to ensure a balance between individual freedom and public safety interests. Further studies are needed, given the methodological limitations of this study.
ABBREVIATIONS
PD – Personality disorder
PSMH – Psychiatry and Safety Measures Hospital
ICD-10 – International Classification and Statistics of
Diseases and Related Health Problems, Revision 10
SCID –II – Structured Clinical Interview for Personality
Disorders Clinical
PANSS – Positive and Negative Symptom Scale –Scale of positive and negative symptoms in schizophrenia
CGI-S – Clinical Global Impression – severity PANSS_EC – excited-component of PANSS PANSS_P – PANSS positive score
PANSS_N – PANSS negative score
PANSS_G – PANSS general psychopathology scale
PANSS_T – PANSS total score
CGI-S – Clinical Global Impression – severity
HCR-20 – Historical Clinical and Risk Management SPSS – Statistical Package for Social Sciences ANOVA – analysis of variance
SD – standard deviation
OT – occupational therapy
REFERENCES
1.Krueger RF. The Alternative DSM-5 Model for Personality Disorders. Medscape 2014.
2.Hart SD. Commentary: The Forensic Relevance of Personality Disorder. J Am Acad Psychiatry Law 2002;30: 510 –12.
3.Huang Y, Kotov R, Girolamo G, Preti A. Angermeyer M at al. DSM–IV personality disorders in the WHO World Mental Health Surveys. Br J Psychiatry 2009;195(1): 46–53.
4.Kent S, Fogarty, M, Yellowlees P. Heavy utilization of inpatient and outpatient services in a public mental health service. Psych Serv
1995;46: 1254–1257.
5.Fazel S, Yu R. Psychotic Disorders and Repeat Offending: Systematic Review and Meta-analysis. Schizophr Bull 2011;37(4): 800-810.
6.***ICD-10. Clasificarea tulburărilor mentale și de comportament, simptomatologie și diagnostic clinic, publicată de OMS. București: Ed. All Educational, 1998.
7.First MB, Gibbon M, Spitzer RL et al. The Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington: American Psychiatric Press, 1997.
8.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13: 261–76.
9.Guy W. Clinical Global Impressions: In: ECDEU Assessment Manual for Psychopharmacology. Revised DHEW Pub. (ADM). Rockville, MD: National Institute for Mental Health, 1976, 218-222.
10.Douglas KS, Guy LS, Weir J. HCR-20 violence risk assessment scheme: Overview and annotated bibliography. Burnaby, Canada: Department of Psychology, Simon Fraser University, 2006. available on- line: www.sfu.ca
11.Adel A, Grimm G, Neil L, Mogge T. Sharp Prevalence of Personality Disorders at a Rural State Psychiatric Hospital. J Rural Community Psychol 2006; E9:1.
12.De Ruiter C, Robert L. Trestman Prevalence and Treatment of Personality Disorders in Dutch Forensic Mental Health Services. J Am Acad Psychiatry Law 2007;35(1): 92-97.
13.Hildebrand M, de Ruiter C. PCL-R psychopathy and its relation to DSM-IV Axis I and Axis II disorders in a sample of male forensic psychiatric patients in the Netherlands. Int J Law Psychiatry 2004;27: 233–48.
14.Timmerman IGH, Emmelkamp PMG. The prevalence and comorbidity of Axis I and Axis II disorders in a group of forensic patients. Int J Offender Ther Comp Criminol 2001;45: 36–149.
15.Stupperich A, Ihm H, Strack M. Violence and Personality in Forensic Patients, Is There a Forensic Patient–Specific Personality Profile? J Interpers Violence 2009;24(1): 209-25.
16.Mosescu M, Stefanescu A. Personality disorders and forensic in- patients, paper at 8th European Congress of International Society for the Study of Personality Disorders, Targu Mures, 2008.
17.Sivaprasad L. Treatment and Outcomes in Secure Care. In: Clark T (ed.). Practical Forensic Psychiatry, Hachette UK, 2011.
18.Devantoy R, Olie JP, Gourevitch R. Risk of homicide and major mental disorders: a critical review. Encephale 2009;35(6): 521-30.
19.Esbec E, Echeburúa E. Violence and personality disorders: clinical and forensic implications, Actas Esp Psiquiatr 2010;38(5): 249-261,
20.Bahlmann M, Preuss UW, Soyka M. Chronological relationship between antisocial personality disorder and alcohol dependence. Eur Addict Res 2002;8: 195-200.
21.Mihailescu LL, Mihailescu R. Variabile clinice și non-clinice ale comportamentului agresiv. Rom J Psychiat. 2007;3(9).
22.Duggan C, Howard RC. The ‘functional link’ between personality disorder and Violence: A critical appraisal. In: M McMurran, RC
Howard (eds.). Personality, personality disorder and violence.
Chichester: Wiley, 2009, 19–38.
23.Johnson SC, Elbogen EB. Personality disorders at the interface of psychiatry and the law: legal use and clinical classification. Dialogues Clin Neurosci 2013;15(2): 203–211.
24.Volavka J, Swanson J. Violent behavior in mental illness: the role of substance abuse. J Am Med Assoc 2010;304(5): 563-4.
25.Moran P, Walsh E, Tyrer P et al. Impact of comorbid personality disorder on violence in psychosis, Report from the UK700 trial. Brit J Psychiat 2003;182: 129 -134
26.Bo S, Abu-Akel A, Kongerslev M et al. The role of co-morbid personality pathology in predicting self-reported aggression in patients with schizophrenia. 2013;54(5): 423-31.
27.Volavka J. Comorbid personality disorders and violent behavior in psychotic patients. Psychiatr Q 2014; 85(1): 65-78. doi: 10.1007/s11126-013-9273-3.
28.Bahorik AL, Eack SM. Examining the course and outcome of individuals diagnosed with schizophrenia and comorbid borderline personality disorder. 2010;124(1-3): 29-35.
29.Laajasalo T, Salenius S, Lindberg N et al. 2011;34(5): 324-30.
30.Volavka J. Violence in schizophrenia and bipolar disorder. Psychiat
Danub 2013; 25(1): 24-33.
31.Cullen AE, Clarke AY, Kuipers E et al. A multi-site randomized controlled trial of a cognitive skills programme for male mentally disordered offenders: social-cognitive outcomes. Psychol Med 2012;42: 557–569.
32.Karterud S, Pedersen G, Bjordal E et al. Day treatment of patients with personality disorders: experiences from a Norwegian treatment research network. J Pers Disord 2003;17(3): 243-62.
33.Völlm B. Assessment and management of dangerous and severe personality disorders. Curr Opin Psychiatry 2009;22(5): 501-6.
34.Fazel S , Zetterqvist J, Larsson H et al. Antipsychotics, mood stabilisers, and risk of violent crime. Lancet 2014. pii: S0140-
6736(14)60379-2.
35.Reid WH, Thorne SA. Personality disorders. In: Simon RI, Tardiff K (eds). Violence Assessment and Management. Washington DC: American Psychiatric Publishing, 2008, 161-185.
36.Warren JI, Burnette M, South SC et al. Personality disorders and violence among female prison inmates. J Am Acad Psychiatry Law 2002;30(4): 502-9.
***




